A telemedicine center (TMZ) enables the care of patients by means of telemedicine. The aim of a telemedicine center is to provide medical diagnostic and therapeutic services across geographical distances as quickly as possible using electronic healthcare services. The development of telemedicine centers has been gaining momentum in Germany over the past few years. The following section explains the potentials that arise – in particular through telemonitoring -, how the processes of telemedical services are defined and which TMZs already exist.
Potential of telemedical services
Telemedicine services for prevention, diagnosis, therapy support, follow-up and aftercare can close the growing gap between treatment needs and current care provision. Telemedicine centers play a central role here, as they support comprehensive and timely patient care. Telemonitoring involves monitoring a patient’s health status via digital communication channels for the purpose of medical diagnostics, therapy and monitoring using external or implanted devices.
Telemonitoring for heart failure
From a medical point of view, early detection of a deterioration in the state of health of heart failure patients and the timely initiation of therapeutic measures make sense. Both are feasible with telemonitoring. Scientific evidence on this is provided by the TIM-HF-2 study1, for example and the IN-TIME study2, which showed a significant reduction in overall mortality and hospitalization time through patient support with highly structured telemonitoring. Avoiding inpatient stays also saves costs. There are several studies3 4 5, that show positive cost effects for telemonitoring of heart failure patients. In particular, costs can be reduced by avoiding re-hospitalizations6.
Telemonitoring for other indications
As with heart failure, it is crucial to recognize a deterioration in health at an early stage in the case of a COVID-19 infection and, if necessary, to initiate measures. However, patients can be monitored at home for as long as possible in order to prevent unnecessary hospital stays and thus the tying up of valuable resources. In a study conducted by Wurzer, Spielhagen et al., around 90% of admitted COVID-19 patients stated that they would have delayed hospitalization further if they had not taken part in the study7. With the help of in-ear sensors, the vital parameters of the study participants were monitored remotely during the illness period and medical care was provided at an early stage if their state of health deteriorated. The TELECOVID study conducted by the Klinikum rechts der Isar (Technical University of Munich) also suggests that telemonitoring using external sensors can be a sensible solution, especially for monitoring COVID-19 patients8.
The potential of telemonitoring is also promising for other indications, for example in the monitoring of breast cancer patients9 or people with COPD.
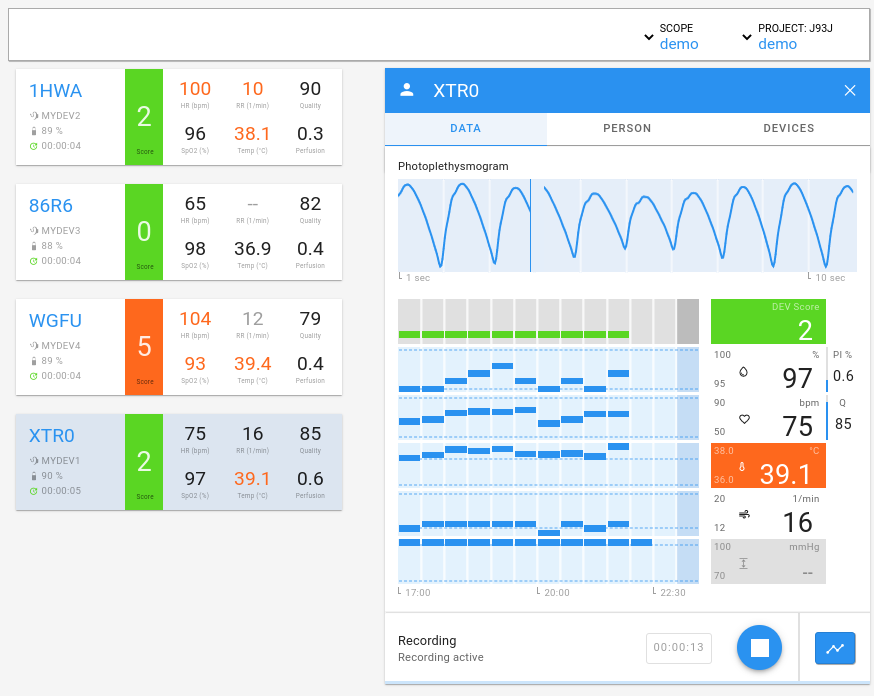
Fig. 1: cosinuss° Health Web.
With telemonitoring, the measured vital data of the patient can be monitored in real time via a dashboard. This example shows a display from the cosinuss° Health dashboard and the detailed view of a patient.
Economic potential of telemonitoring
Currently, telemonitoring is only integrated into standard care for heart failure. However, the BMG’s digitalization strategy envisages making telemonitoring part of digital disease management programmes (DMP). Although implementation is still in its infancy, the economic potential is huge. For example, an analysis by McKinsey10 suggests that the comprehensive introduction of telemonitoring in the German healthcare system could generate an annual potential of EUR 4.3 billion.
The increasing number of selective contracts11, that some health insurance funds have already entered into in limited regions, e.g. for device-supported telemedical care in inpatient care facilities12 or for telemonitoring of blood glucose levels in diabetes patients, also shows that there is a lot of potential in telemonitoring services13.
Telemedicine centers as new service providers
The German Association for Digital Healthcare sees the establishment of telemedicine centers as service providers as crucial to ensuring nationwide healthcare coverage14. Driven by the possibility of EBM billing for telemonitoring in advanced heart failure, which has been in place since 2022, telemedicine centers have been established in recent years (see list below).
The telemedical care of patients requires cooperation between physicians who primarily treat patients (PBA) and make treatment decisions (general practitioners, internists without a specialty, pediatricians, cardiologists, nephrologists or pulmonologists15) and a telemedical center. The billable telemonitoring is carried out via telemetry-capable implanted devices, such as event recorders, pacemakers, implantable cardioverter/defibrillators and implants for cardiac resynchronization or via external sensors, such as blood pressure monitors and body scales, electrocardiograms or other medical devices (e.g. in-ear sensors).
Only qualified cardiologists who meet certain additional requirements can perform the tasks of a TMZ.16
Organizational anchoring of the telemedicine centers
The organizational structure of telemedicine centers, i.e. who performs the telemonitoring service, can be regulated in various ways (see Fig. 2). For example, the TMZ can act as an external service provider. In this case, it is a legally and economically independent company. The TMZ can also be anchored within a hospital. In this case, there is a professional and organizational link between the two entities. As a third form, the TMZ can be operated by a network of doctors consisting of an association of general practitioners and/or specialists in private practice.17
Procedure of telemonitoring with telemedicine centers
The TMZ is responsible for instructing and informing patients about telemonitoring and the use of the devices used, as well as for their technical equipment. The device that records the patient’s vital signs transmits the data to the responsible TMZ. There, the data is stored on an electronic platform and evaluated by medical staff using anamnesis data such as age, gender, concomitant diseases, risk factors and medications. Normally, the patient’s measurements are evaluated on weekdays and, if indicated, also at weekends and on public holidays. In the event of abnormal findings, the “24h/48h hour rule” applies18: the TMZ forwards the alarms to the PBA within 24 hours. The PBA then has 48 hours to inform the patient and initiate treatment. In this way, the aim is to intervene as quickly as possible in order to prevent a worsening of the condition and a possible need for inpatient treatment (see Fig. 1).
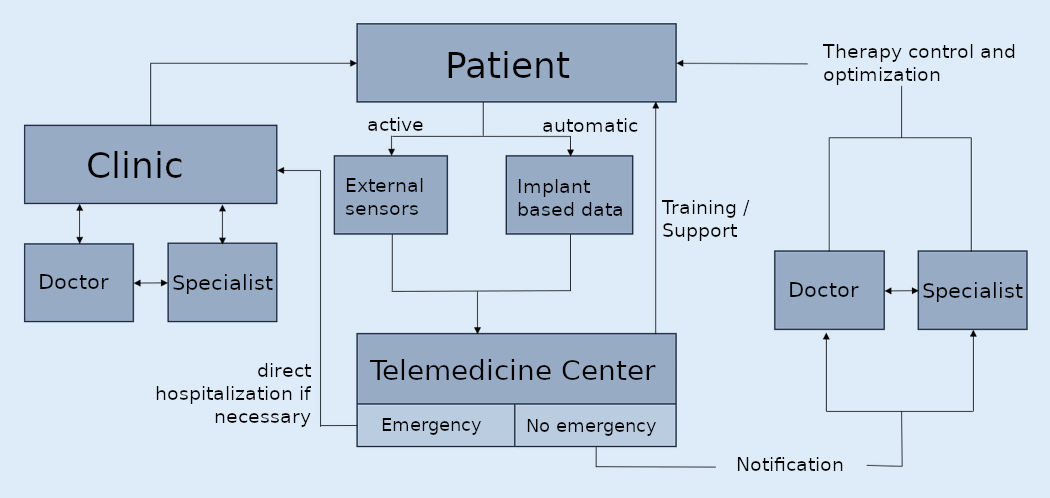
Fig. 2: Information processes in telemedical care.
Nach: Thomas M. Helms, Christian A. Perings et al. (2021): Positionspapier zur Zertifizierung von Telemedizinzentren. In: Kardiologe https://doi.org/10.1007/s12181-021-00522-4, Angenommen: 24. November 2021.
In addition, the Telemonitoring Working Group of the German Society for Cardiology, Cardiovascular Research (DGK) emphasizes that processes within a TMZ should also be strengthened in the future through the use of artificial intelligence (AI)19. With the help of an appropriate algorithm, it is possible, for example, to detect a deterioration in the patient’s state of health at an early stage and make decisions at an early stage as a result (e.g. PolyScore der TELECOVID-Studie).
Billing of telemedical services
As described at the beginning, the range of billable telemonitoring services is currently limited to patients with advanced heart failure (NYHA-II or -III)20. Further telemedical services are to be included in the guidelines and the service catalog of the health insurance companies and thus in standard care in the future. For example, video consultations are already a standard service in statutory health insurance.21
Calculation example based on a fictitious use case
In general, the GOP billing of telemedical services is extrabudgetary and is therefore remunerated at fixed prices. The following is a billing example for the telemedical care of a patient with advanced heart failure for one quarter. In this case example, it is assumed that the patient suffers from advanced heart failure. The primary treating physician (PBA) carries out the examination and determines the indication. As part of the telemedical care, the patient receives an external measuring device to monitor the heart rate. The PBA instructs the patient on how to use the device and on the relevant aspects of self-management. The PBA exchanges information with the responsible TMZ. The tasks of the TMZ include reviewing alerts that require action and clarifying findings that cannot be assessed. The TMZ informs the PBA on the same day of alerts that may require medical action.
Please note: This fictitious example is an attempt to make a calculation that is as close to practice as possible. However, no binding calculations can be made here. Depending on the prevailing conditions, the settlements and therefore the potential amounts may vary significantly. This sample calculation was last updated in June 2022. Individual amounts may therefore have changed in the meantime. You can find the current fee schedule items here: https://www.kbv.de/html/themen_57030.php (Status: April 2024).
Telemedicine care for patients with advanced heart failure
GKV: GOP billing telemonitoring heart failure (general practitioner)
Billings from PBA
- Indication (15 minutes): EUR 7.3222 x 3 = EUR 21.96
- Communication with the responsible TMZ: EUR 14.42
The PBA can bill for telemedicine services in the amount of EUR 36.38 in this example shown.
Billings from TMZ
- Guidance and education: EUR 10.70
- Telemonitoring by means of external measuring devices: EUR 236.59
- Weekend surcharge (external meter): EUR 26.48
- Patient’s equipment (flat rate): EUR 68.00
The TMZ can bill for telemedicine services of EUR 341.77.
In addition, there is an expense reimbursement for the approval processes of contract physicians for health insurance (“bureaucracy cost determination23“) of EUR 26.35.
A detailed list of the individual positions incl. GOP numbers, points and amounts can be found here: Telemonitoring in advanced heart failure reimbursable since 2022
Quality assurance of telemedicine centers
In general, the GOP billing of telemedical services is extrabudgetary and is therefore remunerated at fixed prices. The following is a billing example for the telemedical care of a patient with advanced heart failure for one quarter. In this case example, it is assumed that the patient suffers from advanced heart failure. The primary treating physician (PBA) carries out the examination and determines the indication. As part of the telemedical care, the patient receives an external measuring device to monitor the heart rate. The PBA instructs the patient on how to use the device and on the relevant aspects of self-management. The PBA exchanges information with the responsible TMZ. The tasks of the TMZ include reviewing alerts that require action and clarifying findings that cannot be assessed. The TMZ informs the PBA on the same day of alerts that may require medical action.
Please note: This fictitious example is an attempt to make a calculation that is as close to practice as possible. However, no binding calculations can be made here. Depending on the prevailing conditions, the settlements and therefore the potential amounts may vary significantly. This sample calculation was last updated in June 2022. Individual amounts may therefore have changed in the meantime. You can find the current fee schedule items here: https://www.kbv.de/html/themen_57030.php (Status: April 2024).
Which telemedicine centers already exist?
There are now several telemedicine centers in Germany that can offer and bill telemonitoring services for heart failure. The DGK offers telemedicine centers a certification option. However, DGK certification should not be confused with KV approval for TMZ services. DGK certification certifies that the facility meets the defined criteria for “telemedicine centers”. In order to be able to carry out and invoice telemonitoring for heart failure, approval from the relevant health insurance provider is required. This is granted if the equipment and technical requirements are met in accordance with the quality assurance agreement.24 In the meantime, many GP practices or cardiology practices can also have the telemonitoring of heart failure patients billed via health insurance.
The following is a list of telemedicine centers and providers of telemedicine services in Germany (and Austria).
- Helios Device- und Telemedizinzentrum GmbH, Berlin (D)
- Herz- und Diabeteszentrum Nordrhein-Westfalen: Institut für angewandte Telemedizin (IFAT), Bad Oeynhausen (D)
- Kardio TMZ Rostock, Rostock (D)
- Kardiologisches Telemedizinzentrum Trier, Trier (D)
- KLWS St. Pauls GmbH St. Marien Hospital Lünen + WZAT, Lünen (D)
- Medizinische Universität Innsbruck (Univ.-Prof. Dr. Gerhard Pölzl), in Zusammenarbeit mit dem Landesinstitut für Integrierte Versorgung, Tirol (AT)
- Telemedizin-Zentrum Klinikum rechts der Isar, Technische Universität München, München (D)
- Telemedizincentrum Charité (TMCC), Berlin (D)
- Telemedizinzentrum (TMZ) Kardiologie der Hamburger Asklepios Kliniken, Hamburg (D)
- Telemedizinzentrum der Uniklinik RWTH Aachen, Aachen (D)
- Telemedizinzentrum für Herzinsuffizienz (TMZ) – Telekardiologie Herne, Herne (D)
- Telemedizinzentrum München Klinik Harlaching, München (D)
- Telemedizinzentrum von GIG (Gesellschaft für integrierte Gesundheitsversorgung), Bochum (D)
- Telemonitoringzentrum (TMZ) der Sana Gesundheitszentren Berlin-Brandenburg (SGZ), Berlin-Brandenburg (D)
- ze:roPRAXEN (Kooperation mit SHL Telemedizin Gruppe): Eigenes Telemedizin-Zentrum (TMZ), Metropolregion Rhein-Neckar (D)
Please note: This list does not claim to be exhaustive and is constantly being expanded (last update: April 2024). Are you a telemedicine center in Germany, Austria (or Switzerland) and are not on this list? Please feel free to contact us: info@cosinuss.com.
Provider of infrastructure and services in the field of telemedicine
Further information
- Telemonitoring with cosinuss°: Remote Patient Monitoring
- Telemonitoring bei fortgeschrittener Herzinsuffizienz seit 2022 abrechenbar
This article was originally published on April 5, 2022. It was last updated on April 26, 2024.
Quellen / References
- Köhler F, Köhler K, Deckwart O et al (2018) Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet392:1047–105
- Hindricks G, Taborsky M, Glikson M et al (2014) Implant-based multiparameter telemonitoring of patients with heart failure (IN-TIME): A randomised controlled trial. Lancet384:583–590
- Czypionka, Thomas; Kraus, Markus; Rauer, Eva Susanne; Stegner, Christoph (2022): Telemedizinische Versorgung chronisch kranker Personen – Auswirkungen auf ausgewählte Aspekte der Versorgung am Beispiel von COPD, Diabetes und Hypertonie. Institut für Höhere Studien –I nstitute for Advanced Studies (IHS) https://irihs.ihs.ac.at/id/eprint/6252/1/czypionka-kraus-et-al-2022-telemedizinische-versorgung-copd-diabetes-hypertonie.pdf (Letzter Abruf: 24.4.2024).
- Meisheit, Bernd Christoph et al. (2023): Behandlung aus der Ferne: Warum Telemedizin immer wichtiger wird. SANA Kliniken. https://www.sana.de/newsroom/behandlung-aus-der-ferne-warum-telemedizin-immer-wichtiger-wird/ (letzter Abruf: 26.4.2024).
- Sydow H, Prescher S, Koehler F, Koehler K, Dorenkamp M, Spethmann S, Westerhoff B, Wagner C, Liersch S, Rebscher H, Wobbe-Ribinski S, Rindfleisch H, Müller-Riemenscheider F, Willich SN, Reinhold T. Cost-effectiveness of a non-invasive telemedical interventional management in patients with heart failure: Health Economic Analysis of the TIM-HF2-trial, Clin Res Cardiol. 2021 Dec 11. https://link.springer.com/article/10.1007%2Fs00392-021-01980-2
- Midekke, M. (2009): 15 Chronische Herzinsuffizienz – Kosten reduktion durch Telemedizin. In: Goss, Franz et al.: 2009 Praktische Telemedizin in Kardiologie und Hypertensiologie DOI: 10.1055/b-0034-42342 https://www.thieme-connect.de/products/ebooks/lookinside/10.1055/b-0034-42342
- Wurzer D, Spielhagen P, Siegmann A, Gercekcioglu A, Gorgass J, et al.: “Remote monitoring of COVID-19 positive high-risk patients in domestic isolation: A feasibility study”. PLOS ONE 16(9), 2021.
- M. Baldinger, et al.,“TELECOVID: Remote Vital Signs Monitoring of COVID-19 Risk Patients in Home Isolation With an In-Ear Wearable“ in IEEE Pervasive Computing, vol. 20, no. 02, pp. 58-62, 2021.
- see CO-SI-ONKO
- Biesdorf, Dr. Stefan; Niedermann, Dr. Florian; Sickmüller, Katharina; Tuot, Dr. Kristin (2022): Digitalisierung im Gesundheitswesen: die 42-Milliarden-Euro-Chance für Deutschland. McKinsey & Company. https://www.mckinsey.de/~/media/mckinsey/locations/europe%20and%20middle%20east/deutschland/news/presse/2022/2022-05-24%2042-mrd-euro-chance/220524_mckinsey_die%2042-mrd-euro-chance.pdf
- Carius, Christine (2024): Selektivverträge in der Telemedizin https://www.linkedin.com/pulse/selektivvertr%25C3%25A4ge-der-telemedizin-christine-carius-h1g1c/?trackingId=E9g4%20qWe1t3j%202vBWkVp2w (letzter Abruf: 26.4.2024)
- AOK: https://www.aok.de/pp/nordost/pm/selektivvertrag-fuer-geraetegestuetzte-telemedizinische-versorgung-in-stationaeren-pflegeeinrichtungen/ (letzter Abruf: 26.4.2024)
- iKKBB https://www.ikkbb.de/versicherte/leistungen/im-krankheitsfall/chronische-erkrankungen/diabetesmanagement (letzter Abruf: 26.4.2024)
- POTENZIALE DER TELEMEDIZIN FÜR EINE BESSERE VERSORGUNG NUTZEN (2022): Positionspapier des Spitzenverbands Digitale Gesundheitsversorgung e. V. (SVDGV) https://digitalversorgt.de/wp-content/uploads/2022/02/Positionspapier-Potenziale-der-Telemedizin.pdf
- Kassenärztliche Bundesvereinigung (April 2024): KBV PraxisInfo Telemonitoring bei Herzinsuffizienz. https://www.kbv.de/media/sp/PraxisInfo_Telemonitoring_Herzinsuffizienz.pdf (Letzter Abruf: 24.4.2024)
- Kassenärztliche Bundesvereinigung (2022): Telemonitoring für Patienten mit Herzinsuffizienz startet https://www.kbv.de/html/1150_56619.php (Letzter Abruf: 17.4.2024)
- Thomas M. Helms, Christian A. Perings et al. (2021): Positionspapier zur Zertifizierung von Telemedizinzentren. In: Kardiologe https://doi.org/10.1007/s12181-021-00522-4, Angenommen: 24. November 2021
- Bosch, Ralph; Leonhardt, Volker; Belke, Roberto: Entwicklung, Funktion und Potenzial telemedizinischer Monitoring-Plattformen in der Kardiologie (S. 184). In: McKinsey & Company: Padmanabhan, Pirkka; Redlich, Matthias; Richter, Laura; Silberzahn, Tobias (Hrsg.): E-Health Monitor 2023 | 24.
- Thomas M. Helms, Christian A. Perings et al. (2021): Positionspapier zur Zertifizierung von Telemedizinzentren. In: Kardiologe https://doi.org/10.1007/s12181-021-00522-4, Angenommen: 24. November 2021.
- Prerequisites for the billing of telem. Care are: The patient has heart failure according to NYHA II or NYHA III stage with an ejection fraction < 40%. The patient has an implanted cardiac device (ICD, CRT-P, CRT-D) or has been hospitalized in the past year due to cardiac decompensation. The heart failure is being treated according to the guidelines. There are no identifiable factors that would prevent or jeopardize the transmission of monitoring data or that would hinder the patient’s self-management (https://www.kbv.de/media/sp/2020_12_17_RMvV_37_anerkannt_Telemonitoring_Herzinsuffizienz_BAnz.pdf ).
- Abrechnung der Videosprechstunde gemäß GOÄ (Telemedizin) https://abrechnungsstelle.com/videosprechstunde/ (letzter Abruf: 26.4.2024).
- Can be charged per full five minutes and a maximum of three times in case of illness.
- 2020-12-17_MVV-RL_Telemonitoring-Herzinsuffizienz_TrG.pdf [Internet]. [cited 11. April 2022]. Available at: https://www.g-ba.de/downloads/40-268-7196/2020-12-17_MVV-RL_Telemonitoring-Herzinsuffizienz_TrG.pdf
- Telmedicon – Nur zwei zertifizierte Telemedizinzentren in Deutschland?! https://telmedicon.de/2023/04/17/nur-zwei-zertifizierte-telemedizinzentren-in-deutschland/ (letzter Abruf: 26.4.2024)






