Early Warning Score – Definition and Background
Think of a ward full of patients, some diagnosed with a chronic disease, some under post-operational monitoring. How do care providers decide which patients’ condition needs closest attention? The degree of clinical deterioration can be most accurately predicted by the patients’ vital signs 1. The Early Warning Score (EWS), born in the late 1990s in the UK, is simply a medical guide to quickly evaluate the level of a patient’s clinical deterioration, in both emergency and general care conditions. It is a physiological scoring system, based on the individual values of multiple vital signs.
These are including, but not limited to: 2
- Core body temperature
- Heart rate
- Respiratory rate
- Blood oxygen saturation
- Blood pressure (systolic)
- Level of consciousness.
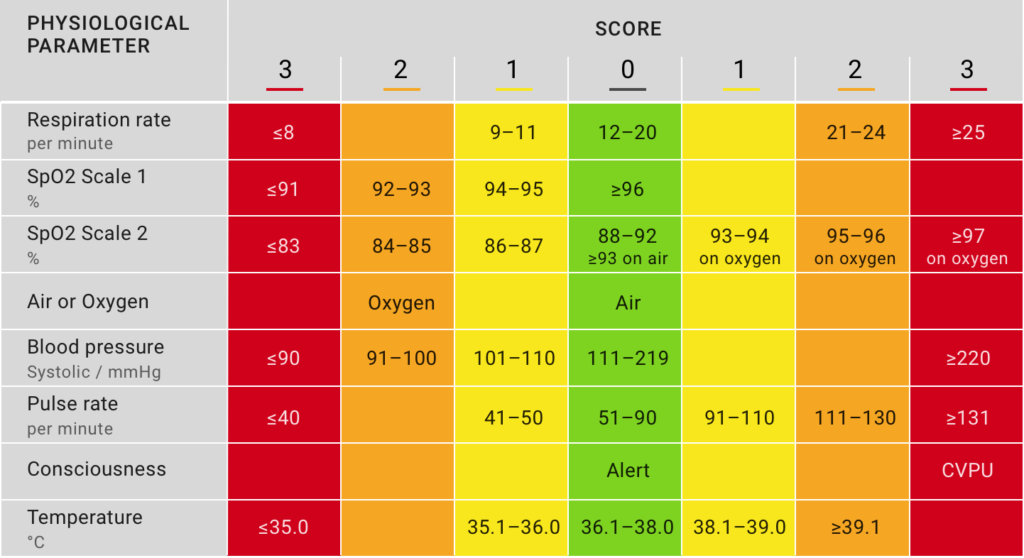
For each vital sign, the deviation from its normal range is assessed and classified into threshold ranges, with individual scores from 0 to 3, according to severity. By combining each vital sign scores, a single aggregate score is eventually generated, constituting the EWS. The EWS itself is then classified mainly into three clinical trigger levels: low (1-4), medium (5-6) and high risk (7 or more). 3 For example, a score of 7 indicates an increased likelihood of admission to intensive care or mortality, while a score of 4 classifies as low clinical risk.
Types of Early Warning Scores
EWS comes in different forms for different patient types and purposes.
Triage Early Warning Score (TEWS)
The Triage Early Warning Score (TEWS) is mostly used in emergency departments to identify and prioritize high-risk patients. 4
Pediatric Early Warning Score (PEWS)
The Pediatric Early Warning Score (PEWS) is designed for patients under 16.
National Early Warning Score (NEWS)
In an attempt to provide a standard national score in the UK, the Royal College of Physicians developed National Early Warning Score (NEWS).2 This score was compared against a number of other EWS protocols and proved to have a high sensitivity in predicting acute mortality 3. The NEWS2 was introduced in 2017, as part of a ‘track and trigger’ system for identifying acutely ill patients, including those with sepsis, in hospitals. NEWS score has been accepted and used outside the UK as well. 1,2
Implementation of Early Warning Score – Where and how is it used?
At the moment, EWS is mostly used for in-hospital patients, to determine the appropriate level of clinical care. The score typically utilizes the current vital sign values, collected manually by nurses, in a paper-based chart, at specified time points. It is important to understand that EWS is not a diagnostic tool, but a facilitator to personalize the monitoring and clinical decision-making around each patient, in a standardized way.
The core principle of EWS is the same all over the world: clinical deterioration can be detected by monitoring the physiological vital signs. An increasing score indicates a need for increased frequency of patient observations or an immediate review by the emergency team (in case of a high score). However, implementation of the EWS protocol is tailored to different parts of the world, to meet the specific needs of different populations and diseases, sometimes including additional parameters, such as urine output 2. Yet, certain parameters play a weighted role to predict mortality within 24 hours 5, which lays emphasis on a standardized approach, in the interest of patient safety.
Wearable technologies and the future of EWS
Digital technologies are rapidly evolving and transforming how we think of healthcare. According to the Forbes article by Bernard Marr 6, big data analytics, artificial intelligence, mHealth, and wearables are among the key technologies that will profoundly impact the healthcare in the 2020s. In near future, we all may have mobile intelligent systems that monitor our vital signs continuously and transmit the data to medical doctors. So that we can take proactive, preventive actions before a high-risk incident, such as cardiac arrest, happens. Indeed, the recently approved Digital Healthcare Act by the German Federal Ministry of Health 7 shows that our regulators are as well convinced of the power of innovative digital solutions in healthcare.
Convenient and effective Monitoring
Early warning score practice can tremendously benefit from wearable digital technologies. A clinical validation study of a wearable, wrist-based device to provide NEWS in a hospital setting 8 demonstrated that, in principle, wearable devices could provide a convenient and reliable method of monitoring.
First of all, wearable sensors enable mobile and frequent, if not continuous, vital sign measurements. This means less susceptibility to omission, and therefore more opportunities to identify clinical decline on time. In fact, a study shows that including vital sign trends over time in the EWS calculation increases the accuracy in identifying critical decline on the wards significantly1. Such devices will also release the clinical staff from the burden of time consuming manual data collection.
Reliable accuracy in data recording
Second, wearable sensors can increase the accuracy of the vital signs data recording, and thus the overall accuracy and predictive power of EWS. To this point, respiratory rate is recognized to be a critical physiological parameter to detect early warning signs of clinical deterioration 9, 10, 11. However, the typically practiced manual observation is highly unreliable 12. Advanced sensor technologies and algorithms, combined with the right wearable design, can effectively solve the accuracy and reliability challenge of vital sign data recording.
Smart proactive healthcare
On top, smart, connected wearable sensors enable automated computation of the EWS, which does reduce not only the risk of a human error, but also the workload of busy clinical staff. Finally, through effective, predictive machine learning algorithms, care providers can receive timely notifications on the patient’s condition and proactively step in, before there is a severe escalation.
All that being said, currently available medical-grade wearables in the market can monitor only few of the key vital signs. Many of them are wrist-based wearables, what makes the vital sign data accuracy questionable, compared to in-ear measurements.
How can cosinuss° make a difference in EWS?
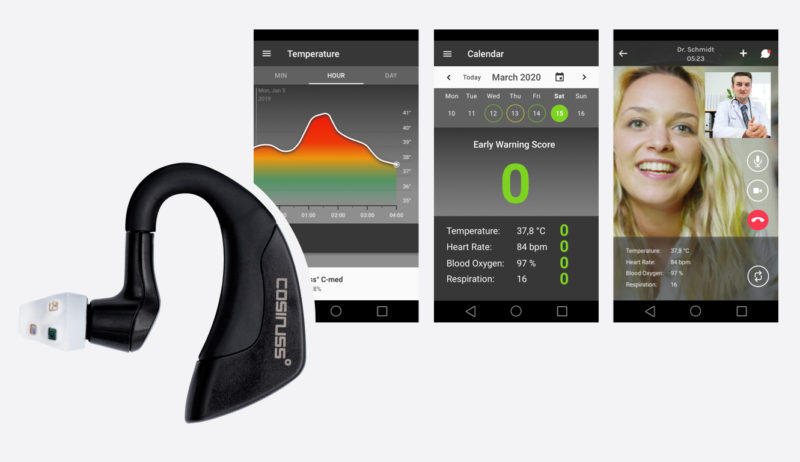
cosinuss° provides the unique combination of mobile, continuous monitoring of four key components of EWS, in a single device, with high accuracy. The in-ear wearable sensor measures Heart Rate, Core Body Temperature, Blood Oxygen Saturation and Respiratory Rate, in real-time, providing the health practitioner with a complete picture of the patient’s physiological condition, anytime, anywhere.
Are you interested in a medical-grade wearable sensor, which can feed accurate vital signs data to your EWS software? Or do you prefer to have a complete EWS solution that would help you improve patient outcomes? Please get in touch.
We are just at the beginning of a new era in patient monitoring. Let’s shape it together!
Contact Person:
Dr.-Ing. Johannes Kreuzer, CEO
E-mail: info@cosinuss.com
Telemedicine Center / Center for telehealth
A telemedicine center (TMZ) enables the care of patients by means of telemedicine. The aim of a telemedicine center [...]
Vital data-enhanced evacuation system for the military
Cooperation between drone manufacturer AVILUS and medical technology company cosinuss° Munich/Ismaning, 29.01.2024 - In the event of serious [...]
Sepsis: Early Detection & Aftercare
Higher chances of survival thanks to sensor technology In case of sepsis (colloquially blood poisoning), every hour counts. [...]
Quellen / References
- The value of vital sign trends for detecting clinical deterioration on the wards (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4834231/pdf/nihms764868.pdf)
- A Review of Early Warning Systems for Prompt Detection of Patients at Risk for Clinical Decline.
- Royal College of Physicians, National Early Warning Score (NEWS), 13 May 2015 (https://www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news)
- “An evaluation of the Triage Early Warning Score in an urban accident and emergency department in KwaZulu-Natal” (https://www.ajol.info/index.php/safp/article/viewFile/102712/92979)
- ViEWS–Towards a National Early Warning Score for Detecting Adult Inpatient Deterioration (https://pubmed.ncbi.nlm.nih.gov/20637974-views-towards-a-national-early-warning-score-for-detecting-adult-inpatient-deterioration/)
- “The 9 Biggest Technology Trends That Will Transform Medicine And Healthcare In 2020” (https://www.forbes.com/sites/bernardmarr/2019/11/01/the-9-biggest-technology-trends-that-will-transform-medicine-and-healthcare-in-2020/#1b7caddd72cd)
- Driving the digital transformation of Germany’s healthcare system for the good of patients (https://www.bundesgesundheitsministerium.de/digital-healthcare-act.html)
- ChroniSense National Early Warning Score Study (CHESS): a wearable wrist device to measure vital signs in hospitalised patients—protocol and study design https://bmjopen.bmj.com/content/9/9/e028219
- Elliot, Malcolm, et al. “Critical care: The eight vital signs of patient monitoring.” British journal of nursing (Mark Allen Publishing) 21(10):621-5
- Baker SP, O’Neill B, Haddon W Jr., Long WB. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma Inj Infect Crit Care. 1974;14(3):187–196.
- Fieselmann JF, Hendryx MS, Helms CM, et al. Respiratory rate predicts cardiopulmonary arrest for internal medicine patients. J Gen Intern Med 1993; 8: 354-360.
- Mok, W et al. Attitudes towards vital signs monitoring in the detection of clinical deterioration: scale development and survey of ward nurses. Int J Qual Health Care (2015) 27 (3): 207-213. (https://www.ncbi.nlm.nih.gov/pubmed/25888564)