Respiration rate
Synonyms and abbreviations: Respiratory rate (RR), breathing rate.
Respiration rate is the number of breaths per unit of time (usually per minute). It affects heart rate, blood pressure and oxygen saturation. The respiratory rate, like all vital signs, depends on individual variations and external influences. It is an important parameter for assessing the state of health.
Overview
| Unit | Breaths per minute (min-1) |
| Normal values (approx.) | Newborns 30-50 Infants 20-40 Toddlers 20-30 Children 18-24 Adults 12-16. |
| Measurement methods | Manual Spirometry Capnometry ECG/impedance pneumography Photoplethysmography (PPG) |
Definition: What is the respiration rate?
Respiration rate or respiratory rate is the number of breaths per unit of time (usually one minute).1
Respiratory rate, tidal volume & respiratory minute volume
Both respiratory rate and tidal volume depend on age and body size. The tidal volume describes the amount of inhaled air per breath. On average, it is about 500 to 1000 ml for an adult. The rule of thumb for calculating the tidal volume is: Body weight in kg × 10 to 15. The product of respiratory rate and tidal volume is called respiratory minute volume and indicates the amount of air exchange per minute. This is about 7 to 14 l for a healthy adult, but can increase to 80 l during heavy physical exertion and to 120 l during extreme exertion.2
Respiration rate: normal values & deviations
Depending on various individual influencing factors, a healthy adult breathes about 12 to 16 times per minute at rest. The number of breaths per minute varies depending on age, among other factors. In newborns through infancy, breathing frequencies sometimes vary considerably between age groups:
- Premature baby: approx. 50-60 breaths per minute
- Newborn (born mature): 30-50 breaths per minute
- Infant: 20-40 breaths per minute
- Toddler: 20-30 breaths per minute
- Child (6 years and older): 18-24 breaths per minute
- Adult: 12-16 breaths per minute3
From the age of 30, normal values of respiratory rate remain largely constant.4
Increased respiratory rate
Increased respiratory rate can result from a variety of causes, which may be harmless or pathological (for more information, see “What influences respiration rate“).
Tachypnea
A respiratory rate of about 20 per minute or more is referred to as tachypnea. It occurs with increased oxygen demand. The depth of breathing can be reduced, the same or increased with an increased respiratory rate. Causes of tachypnea can be physical exertion (e.g. sports), various diseases or stress.5 6
Hyperventilation
In hyperventilation, too much carbon dioxide is exhaled by breathing too quickly and/or deeply: the CO2 partial pressure drops and at the same time the pH value of the blood rises. This can result in symptoms such as tachypnea, muscle cramps (“pawing”/Obstetrician’s hand due to cramping of the muscles of the forearm and hands), sensory disturbances, dizziness, and anxiety. Causes of hyperventilation can arise from anxiety, stress or excessive physical exertion, as well as from various diseases.7 8
Decreased respiratory rate
A reduced respiration rate can have various causes. Both physiological and pathological factors are possible (for more information, see ” “What influences respiration rate“).
Bradypnea
If the respiratory rate falls below ten breaths per minute at rest, this is called bradypnea.9 A non-pathological form of bradypnea occurs during sleep and deep relaxation. Pathological causes of slowed breathing may include damage to the central nervous system (e.g. traumatic brain injury), metabolic disorders (e.g. hypothyroidism), or medications (e.g. opiates, benzodiazepines).10
Hypoventilation
In hypoventilation, there is insufficient ventilation of the lungs, in that there is too little exhalation of carbon dioxide.11 In this case, the oxygen partial pressure decreases while the arterial CO2 partial pressure increases at the same time. The cause may be a disturbed ventilation of the lungs, e.g. caused by rib fractures or neuromuscular diseases. A disorder of respiratory control can also be the cause of hypoventilation. This occurs, for example, in central sleep apnea syndrome or in severe obesity (obesity hypoventilation syndrome).12 As a result of hypoventilation, there may be an increased carbon dioxide content in the blood (hypercapnia), oxygen deficiency (hypoxemia), as well as hyperacidity of the blood (respiratory acidosis).13
Dyspnea
Dyspnea is the subjective sensation of shortness of breath or difficult breathing. Affected persons have the feeling that they no longer get enough air. Dyspnea can be divided into different categories related to physical exertion (exertion-independent vs. non-exertion-independent), body position (position-independent vs. position-independent), or the type of onset of dyspnea (sudden vs. slow). Many different pathological, physiological as well as psychological factors can be considered as causes, including:
- Pulmonary diseases (e.g. bronchial asthma, COPD, pulmonary embolism, pneumonia).
- Heart disease (e.g. heart failure, myocardial infarction)
- Diseases of the skeleton (e.g. rib fracture)
- Diseases of muscles and nerves (e.g. ALS)
- Psychological factors (e.g. depression, anxiety disorder)
- Other causes, such as obesity14 15
Orthopnea
Excursion: Breathing & Breathing Regulation
Breathing is divided into external and internal respiration. It is a vital process in which our lungs bring oxygen (O2) into the blood and remove carbon dioxide (CO2) (external respiration). In this way, a constant exchange of gases takes place. Depending on the point of entry of the inhaled air, a distinction can be made between mouth and nose breathing.18 Internal respiration refers to cellular respiration (aerobic energy production in humans).19
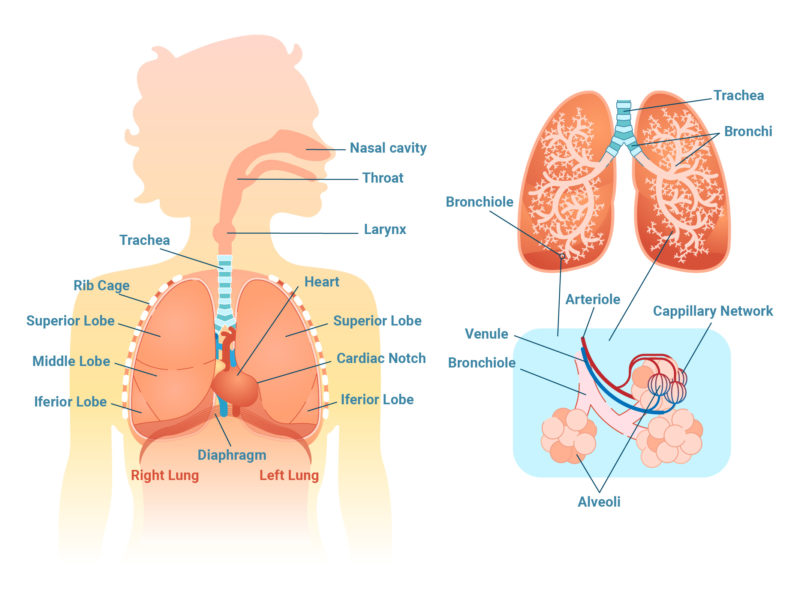
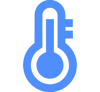
Fig. 1: Organs and body parts involved in external respiration.
External respiration
The aim of external respiration or lung respiration is to supply the body’s cells with oxygen and to release carbon dioxide. External respiration consists of inhalation (inspiration, active) and exhalation (expiration, passive), which can be divided into four steps: 20
- The thorax rises and the diaphragm contracts.
- The inhaled air thus flows into the lungs.
- The respiratory muscles relax again.
- The lungs follow their aspiration to collapse (as far as the thorax allows) and air flows out of them.
The following happens in detail: The inhaled, oxygen-rich air flows into the trachea via the mouth, nose and throat. At the same time, it is warmed, moistened and purified. The air then flows further into the bronchi, bronchioles and finally into the alveoli, which are surrounded by a network of very thin blood vessels (capillaries). Here, gas exchange takes place across the alveolocapillary membrane by diffusion. Inside the alveoli, there is a higher partial pressure of oxygen and a lower partial pressure of carbon dioxide than in the blood. Due to this pressure gradient, oxygen (O2) is absorbed into the blood of the pulmonary circulation (binding to hemoglobin) and at the same time carbon dioxide diffuses from the blood into the alveoli. Via the blood circulation, the oxygen-loaded hemoglobin is transported into the tissues and cells. The carbon dioxide (CO2) produced there by metabolic processes in turn returns to the lungs via the blood and is then exhaled into the environment.21 22 23 24 25
Fig. 2: Gas exchange between lungs and bloodstream.
Briefly explained: O2 and CO2 partial pressure
Partial pressure refers to the respective partial pressure of the individual gases within a gas mixture. For example, the air in our atmosphere is composed of the different gases nitrogen (N2), oxygen (O2) and carbon dioxide (CO2) as well as water vapor (H2O). Each of these gases is present in the gas mixture “air” in a certain proportion and has an individual pressure. When added together, the individual partial pressures of the gases and water vapor result in the total pressure of the gas mixture.
Different partial pressures of the gases are also present in the blood. During respiration, the different partial pressures of O2 and CO2 within the alveoli and arteries are particularly relevant. The difference in the partial pressures of O2 and CO2 ensures that gas exchange between the lungs and blood can take place by diffusion, since the gas particles each move toward the pressure gradient and strive for pressure equalization.26 27
Internal respiration (cellular respiration)
Internal respiration or cellular respiration describes the oxygen-dependent metabolic processes within the body’s cells (aerobic energy production). For their energy supply, our cells take up glucose, which is completely broken down into carbon dioxide and water in the cell plasma and mitochondria. The aim is to provide energy in the form of adenosine triphosphate (ATP) with the help of oxygen, among other things. This is necessary for all metabolic processes in our body. Cellular respiration includes glycolysis, the citrate cycle, and the respiratory chain.28
Breathing regulation: control & adaptation
The regulation and control of our breathing takes place in the respiratory center. This is located in the medulla oblongata, an important regulatory and reflex center located in the continuation of the spinal cord in the brain area. Breathing is controlled automatically in the respiratory center, but it is the only basic automatic function of our body that can be influenced voluntarily (for example, when speaking, singing, and holding one’s breath).
Several groups of neurons are located in the medulla oblongata. Through a complex interplay of these respiratory neurons, our rhythmic activity of inhaling and exhaling takes place. The neurons promote and inhibit each other (interplay between inspiratory and expiratory neurons). In this way, a basic breathing rhythm is made possible, which can be adapted to changing needs and conditions by higher brain centers and other areas of the body. This happens, for example, during sports: in order to meet the increased oxygen demand, the body has to breathe faster. Corresponding signals are transmitted to the respiratory center in the medulla oblongata via special mechanoreceptors in the joints and muscles.
In detail, involuntary respiratory regulation is influenced primarily by the carbon dioxide content, the pH value and the oxygen content of the blood. The most important role, however, is played by the carbon dioxide content. If the various receptors in the body measure a high level of carbon dioxide (CO2) in the blood, the respiratory center increases the respiratory rate so that the excess CO2 in the alveoli can be released into the air we breathe. If, on the other hand, the CO2 concentration is too low, the respiratory rate is reduced.
The oxygen content in the blood, on the other hand, has less influence on automatic respiratory regulation. Adaptation reactions of the body only take place when the oxygen content drops drastically.
In addition to the respiratory neurons mentioned above, various sensors and receptors as well as influences from higher areas of the central nervous system (emotions or reflexes, e.g. coughing, sneezing, yawning and swallowing) play a role in involuntary respiratory regulation. Sensors and receptors that sense respiratory stimuli and transmit them to the respiratory center include chemosensors (e.g. in the aorta, brainstem), mechanosensors (lungs, respiratory muscles), sensors for deep sensitivity of the locomotor system, thermosensors (skin), and hormone receptors.29 30 31 32 33
Thanks to the ability to control our breathing muscles at will, we can consciously change our breathing. This can be used, for example, for certain breathing techniques in sports or when relaxing. However, this control is limited in the case of stronger fluctuations in the concentrations of carbon dioxide, oxygen or a change in the blood pH value.34
What influences the respiration rate?
Many different factors can influence the breathing rate. In addition to pathological causes, physiological and psychological influences as well as changing environmental conditions also play a role.
Respiratory rate during sleep
During sleep, our breathing changes fundamentally, and so does our breathing rate, so that a healthy adult breathes an average of 12 to 16 times per minute (breathing at rest). During the waking state, breathing is mainly controlled by external influences. During sleep, on the other hand, breathing is essentially regulated by metabolism, with special “pacemakers” inside the body (e.g. baroreceptors) being predominantly active.
Since respiratory minute volume and respiratory rate are reduced during sleep, arterial carbon dioxide increases and arterial oxygen partial pressure decreases. At the same time, the airway resistance of the upper airways increases and the natural protective reflex of the lungs (protection against over-expansion of the lungs during inhalation35) decreases.
Breathing rate and depth vary depending on the sleep phase. Thus, during REM sleep there is an increased variability of respiratory rate and depth of breath.36 37 38
In addition to non-diseased changes in our breathing during sleep, there are several sleep-related breathing disorders. These can have various causes:
- Narrowing of the upper airway due to slackening of the muscles (obstructive sleep apnea).
- Central sleep apnea, which is due to a disorder of the respiratory center.
- Hypoventilation syndrome, for example, due to severe obesity, muscular diseases, severe chronic lung diseases or severe curvatures of the spine39
Respiration rate in women and men
The breathing rate of women and men usually differs due to anatomical factors. Women have an average respiratory rate of 14 to 18 and men of 12 to 16.
On the one hand, the differences come from the volume of the upper body (thoracic volume): for example, the female thorax has an average volume of 4 liters, while the male thorax has an average volume of 5 liters. Secondly, there is a difference in breathing type between the sexes. Whereas in women chest breathing is predominant at rest, in men it is abdominal breathing. Furthermore, the respiratory tract is smaller in women than in men (nasal cavity, trachea, bronchi). The lungs also have a different volume on average: In women, this is approx. 4.5 to 5 liters (approx. 1.6% of total body weight) and in men approx. 6.5 to 7 liters (approx. 1.8% of total body weight).40 41 42
Respiratory rate in babies and children
Because infants have a higher basal metabolic rate and, consequently, higher oxygen consumption at rest, they breathe much faster than older children and adults. In addition, the respiratory rate is increased compared to adults due to various anatomical differences.43
Respiratory rate during sport
During sports, our muscles need more oxygen and energy. To ensure this, the respiration rate increases. While we breathe about 12 to 16 times per minute at rest, the breathing rate can increase to 40 to 50 during physical exertion.44 At rest, about two percent of the oxygen taken in is needed for the contraction work of the respiratory muscles. During sport, this value can increase tenfold.45
Regular endurance sports have positive effects on our breathing: The gas exchange surface in the lungs increases. This optimizes respiratory processes and improves lung function overall. Among other things, the respiratory frequency decreases and the tidal volume increases.46 47
Influence of posture on breathing
The body posture we adopt can also have an influence on our breathing. For example, the volume of the lungs is smaller when lying down than when sitting. The reason for this is the changed position of the diaphragm: when lying down, it is pushed upward by the abdominal organs. In addition, there is more blood in the vessels of the chest when lying down, which also restricts the expansion of the lungs. In addition, the diaphragm does most of the inhaling while lying down, so that the abdomen in particular rises (abdominal breathing). In the upright position, the chest tends to expand during inspiration (thoracic breathing).48
Breathing and psyche
On the one hand, our breathing can be influenced by our psyche. On the other hand, restrictions or changes in our breathing can in turn trigger anxiety and stress. Thus, when we are anxious, certain signals from the amygdala located in the brain are sent to our respiratory center, whereupon the breath becomes shallower and faster. The resulting changes in breathing, up to and including (perceived) breathlessness, can in turn generate or intensify strong feelings of anxiety. The resulting continued or even more rapid and flattened breathing again reinforces the symptom of shortness of breath – a vicious circle develops. However, this mechanism can be counteracted by conscious deep and slow inhalation and exhalation. Through slow breathing, feelings of anxiety can thus be reduced again to a certain extent.49
Influence of diseases on the respiratory rate
Various diseases can have an influence on the respiratory rate and either slow it down or increase it.
Highly increased, rapid breathing (tachypnea) can be caused, for example, by fever or due to various heart and lung diseases.50
A strongly slowed breathing (bradypnea) can be caused by damages of the central nervous system (e.g. craniocerebral trauma), metabolic diseases (e.g. hypothyroidism) or drugs (e.g. opiates, benzodiazepines).51
If there is a subjective sensation of difficult breathing (dyspnea), the causes may include the following diseases:
What does respiratory rate indicate?
Respiratory rate, along with other vital signs such as pulse rate and oxygen saturation, is an important indicator for assessing health. Thus, deviations of the normal respiratory rate upwards or downwards can indicate various diseases.54
Disturbances in the body that cause hypoxemia (lack of oxygen in the blood) or hypercapnia (increased CO2 content in the blood) can be detected by measuring the respiratory rate. Altered respiratory rate is also a common feature before serious deterioration of health and subsequent cardiac arrest.55 Especially in the case of diseases affecting the lungs or metabolism, the respiratory rate can serve as a tool for assessing the degree of severity.56 This applies, for example, to diseases such as bronchial asthma, heart failure, pulmonary embolism, and sepsis (“blood poisoning”).57
A study published in 2014 found that there appears to be a correlation between the level of respiratory frequency and mortality in patients with pneumonia. The researchers found that the higher the respiratory rate during hospitalization, the higher the mortality.58
According to a study published in 2020, nocturnal respiratory rate can predict whether implantable cardioverter defibrillators (ICDs) have a preventive effect. For example, in certain diseases of the heart muscles (cardiomyopathy), attempts are often made to prevent dangerous arrhythmias with the help of such ICDs. However, the researchers found that patients with a comparatively high nocturnal respiratory rate (≥ 18 breaths/min) had no survival benefit from an ICD.59
Maximum ventilation volume (MVV)
The respiratory threshold is the maximum respiratory rate of a person. This can be used to assess the respiratory muscles and any respiratory disorders that may be present. The maximum ventilation volume is measured with the aid of a spirometer, in which the patient breathes at his/her maximum possible speed for approx. ten seconds.60
Respiration rate measurement
How to measure respiration rate?
Breathing rate can be measured either manually (on oneself or someone else) or using various devices and physiological principles.
Manual: How to calculate respiration rate
To determine the respiratory rate in yourself or another, the following steps are indicated:
- Before taking the measurement, place a watch with a second display in a clearly visible position.
- First, come to rest for about five minutes (e.g. sit quietly on a chair or lie in bed).
- Place a flat hand where you can best feel your breathing (e.g. stomach or chest). If someone else’s respiration rate is being measured, the rising and falling of the chest or abdomen can also be observed.
- Count the breaths over one minute. From this, the breaths per minute are obtained.61
Although this type of respiratory rate measurement can be very inaccurate depending on the user, it is nevertheless frequently used in clinical practice today.62
Spirometry
Spirometry (“small lung function”, spirare (lat.): to breathe) can be used to measure the respiratory rate. The main function of this examination method is to record the functional state of the lungs by measuring the lung or tidal volume.
During the examination, the patient breathes through a mouthpiece into the so-called “spirometer”. The nose is closed with a clip. The spirometer measures the volume of air inhaled and exhaled, as well as the velocity of the exhaled air. The volumes of air moved during these breaths are mapped graphically and can thus be assessed.63 64 Although this method is very accurate and it can be used to measure several respiratory parameters simultaneously, it affects the patient’s natural breathing and is unsuitable for continuous measurement of respiratory rate.65
Capnometry
Capnometry is used to measure the level of carbon dioxide in a patient’s exhaled air. It is often used in anesthesia or for monitoring ventilated patients. Capnometry can also be used to measure respiratory rate. This form of measurement has high accuracy and is also suitable for continuous measurement of respiratory rate. However, it is uncomfortable for the patient to use and special equipment is needed to analyze the recorded data.66
ECG / Impedance pneumography
An ECG (electrocardiogram) measures the electrical activity of the heart using electrodes attached to the skin. The ECG electrodes can also be used to determine the respiratory rate. This is done by means of so-called impedance pneumography. As we inhale and exhale, the volume of the chest (thorax) increases and decreases. During the increase in volume, the alternating current resistance (impedance) of the thorax increases, and during the decrease in volume, it decreases. With the help of two electrodes placed on the thorax, these changes in impedance can be measured. The fluctuations recorded in this way are displayed on a monitor as an impedance pneumogram (“breathing curve”). From this, the respiratory rate can be determined. A disadvantage of this method is that the signal is very susceptible to motion artifacts. Thus, every movement of the body influences the thoracic impedance.67 68
Rotation rate and acceleration sensors
Another method of measuring the respiratory rate is based on the detection of movements and volume changes that can be observed externally in the chest or abdomen during breathing. For example, a chest strap equipped with a 3-axis gyroscope and acceleration sensors can be used to detect the angular changes caused by the breathing movements and determine the respiratory rate.69
Photoplethysmography (PPG sensor)
Photoplethysmography (PPG) can be used to determine pulse rate and oxygen saturation (SpO2). Respiratory rate can also be extracted from the captured PPG signal and with the help of algorithms. The PPG sensor has either one green LED or two LEDs, one red and one infrared. This light is alternately sent into the tissue (e.g. skin on the wrist or in the ear canal). A photodiode receives the light that has been reflected or not absorbed by the tissue and converts this information into electric current. The current is converted by a transimpedance amplifier (TIA) into an electrical voltage, which in turn can be digitized. As respiration influences variations in venous return, stroke volume and arterial blood pressure, the respiratory rate can be derived from the measured PPG curves by means of frequency analysis.70 71 72
How does cosinuss° measure vital signs?
Author and reference information
About the author
 |
Dr.-Ing. Johannes Kreuzer is co-founder and managing director of cosinuss°. He studied electrical engineering with a focus on medical electronics at TUM (Technical University of Munich, Germany). |
Quellen / References
- Atemfrequenz, www.pschyrembel.de (Abruf: 5.1.2021)
- Mathias D.(2018): Ausdauersport und Lunge. In: Fit und gesund von 1 bis Hundert. Springer, Berlin, Heidelberg https://doi.org/10.1007/978-3-662-56307-6_61
- Atemfrequenz, www.pschyrembel.de (Abruf: 4.2.2021)
- Atemfrequenz, flexikon.doccheck.com (Abruf: 5.1.2021)
- Tachypnoe, www.pschyrembel.de (Abruf: 5.2.2021)
- Tachypnoe, flexikon.doccheck.com (Abruf: 5.1.2021)
- Hyperventilation, flexikon.doccheck.com (Abruf: 5.1.2021)
- Atemfrequenz, flexikon.doccheck.com (Abruf: 5.1.2021)
- Atemfrequenz, flexikon.doccheck.com (Abruf: 5.1.2021)
- Bradypnoe, www.pschyrembel.de (Abruf: 7.1.2021)
- Atemfrequenz, flexikon.doccheck.com (Abruf: 5.1.2021)
- Hypoventialtion, www.pschyrembel.de (Abruf: 7.1.2021)
- Hypoventilation, flexikon.doccheck.com (Abruf: 7.1.2021)
- Dyspnoe, flexikon.doccheck.com (Abruf: 7.1.2021)
- Dyspnoe, www.pschyrembel.de (Abruf: 7.1.2021)
- Atemfrequenz, flexikon.doccheck.com (Abruf: 5.1.2021)
- Orthopnoe, flexikon.doccheck.com (Abruf: 7.1.2021)
- Atmung: Was passiert beim Atmen?, www.lungeninformationsdienst.de (Abruf: 18.1.2021)
- Atmung, www.pschyrembel.de (Abruf: 7.1.2021)
- Die Physiologie der Atmung, www.lecturio.de (Abruf: 18.1.2021)
- Die Physiologie der Atmung, www.lecturio.de (Abruf: 18.1.2021)
- Atmung: Was passiert beim Atmen?, www.lungeninformationsdienst.de (Abruf: 18.1.2021)
- Chrobak, Franziska (2915): Untersuchung zur Regelmäßigkeit der Atmung im Schlaf, Medizinische Fakultät der Friedrich-Schiller-Universität Jena www.db-thueringen.de (Abruf: 19.1.2021)
- Atmung, www.pschyrembel.de (Abruf: 7.1.2021)
- Gasaustausch, flexikon.doccheck.com (Abruf: 19.1.2021)
- Partialdruck, www.pschyrembel.de (Abruf: 4.2.2021)
- Gastransport im Blut, www.amboss.com (Abruf: 5.2.2021)
- Atmung, www.pschyrembel.de (Abruf: 11.1.2021)
- Wie wird die Atmung gesteuert? www.lungeninformationsdienst.de (Abruf: 19.1.2021)
- Chrobak, Franziska (2915): Untersuchung zur Regelmäßigkeit der Atmung im Schlaf, Medizinische Fakultät der Friedrich-Schiller-Universität Jena www.db-thueringen.de (Abruf: 19.1.2021)
- Atemfrequenz, flexikon.doccheck.com (Abruf: 5.1.2021)
- Atemzentrum, flexikon.doccheck.com (Abruf: 5.1.2021)
- Atemregulation, www.pschyrembel.de (Abruf: 5.1.2021
- Atemzentrum, flexikon.doccheck.com (Abruf: 5.1.2021)
- Hering-Breuer-Reflex, flexikon.doccheck.com (Abruf: 19.1.2021)
- Chrobak, Franziska (2915): Untersuchung zur Regelmäßigkeit der Atmung im Schlaf, Medizinische Fakultät der Friedrich-Schiller-Universität Jena www.db-thueringen.de (Abruf: 19.1.2021)
- Schäfer, T., Schläfke, M.E. (1997): Zusammenspiel von Schlaf und Atmung: Untersuchungen zur Atmungsregulation im Schlaf. Somnologie 1, 21-26 https://doi.org/10.1007/s11818-997-0006-04 (Abruf: 19.1.2021)
- Chrobak, Franziska (2915): Untersuchung zur Regelmäßigkeit der Atmung im Schlaf, Medizinische Fakultät der Friedrich-Schiller-Universität Jena www.db-thueringen.de (Abruf: 19.1.2021)
- Schlafbezogene Atmungsstörungen, www.schlafmedizin-essen.de (Abruf: 19.1.2021)
- Atmung der Frau, ruhr-uni-bochum.de (Abruf: 5.1.2021)
- Dominelli, Paolo B. et. al (2018): Sex differences in large conducting airway anatomy. Journal of Applied Physiology 125: 960–965, journals.physiology.org (Abruf: 19.1.2021)
- Dominelli, Paolo B. et. al (2019): Sex Differences in the Pulmonary System Influence the Integrative Response to Exercise, Exercise and Sport Sciences Reviews: July 2019 – Vol 47, Issue 3, p 142-150 doi: 10.1249/JES.0000000000000188
- Atemphysiologie bei Säuglingen, Kindern und Jugendlichen, www.springermedizin.de (Abruf: 18.1.2021)
- Godehardt, Katja (2017): Referenzwerte gesunder Probanden für ventilatorische Parameter und das Atemäquivalent in Ruhe und unter Belastung auf dem Laufbandergometer im Alter von 4 bis 74 Jahren, Universitätsklinik der Ruhr-Universität Bochum, https://d-nb.info/115430812X/34 (Abruf: 18.1.2021)
- Mathias D. (2018): Ausdauersport und Lunge. In: Fit und gesund von 1 bis Hundert. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-56307-6_61
- Mathias D. (2018): Ausdauersport und Lunge. In: Fit und gesund von 1 bis Hundert. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-56307-6_61
- Atmung & Belastung, physiologie.medunigraz.at (Abruf: 5.1.2021)
- Gückler, Julia Nathalie (2016): Einfluss der Körperhaltung auf die Aktivierung der Atemmuskulatur im prolongierten Weaning. Klinik für Pneumologie der Albert-Ludwigs-Universität Freiburg i.Br., freidok.uni-freiburg.de
- Atmung und Psyche – vom Wechselspiel zwischen Lunge und Hirn, www.lungenaerzte-im-netz.de (Abruf: 19.1.2021)
- Tachypnoe, flexikon.doccheck.com (Abruf: 5.1.2021)
- Bradypnoe, www.pschyrembel.de (Abruf: 7.1.2021)
- Dyspnoe, flexikon.doccheck.com (Abruf: 7.1.2021)
- Dyspnoe, www.pschyrembel.de (Abruf: 7.1.2021)
- Gesundheit mit Hilfe der Atemfrequenz untersuchen? www.lungeninformationsdienst.de (Abruf: 18.1.2021)
- Liu H, Allen J, Zheng D, Chen F. (2019): Recent development of respiratory rate measurement technologies. Physiological Measurement. Aug 2;40(7):07TR01. doi: 10.1088/1361-6579/ab299e.
- Strauss R, Ewig S, Richter K, König T, Heller G, Bauer T: The prognostic significance of respiratory rate in patients with pneumonia—a retrospective analysis of data from 705 928 hospitalized patients in Germany from 2010–2012. Dtsch Arztebl Int 2014; 111: 503–8. DOI: 10.3238/arztebl.2014.0503 /Abruf: 18.1.2021)
- Atemfrequenz: Unterschätzter Parameter?, www.coliquio.de (Abruf: 18.1.2021)
- Strauß R, Ewig S, Richter K et al. (2014): The prognostic significance of respiratory rate in patients with pneumonia – a retrospective analysis of data from 705.928 hospitalized patients in Germany from 2010–2012. Deutsches Ärzteblatt; 111: 503-508, https://www.aerzteblatt.de/int/archive/article/161152 (Abruf: 19.1.2021)
- Dommasch M, Steger A, Barthel P, et al. and The EU-CERT-ICD investigators: Nocturnal respiratory rate predicts ICD benefit: A prospective, controlled, multicentre cohort study. EClinicalMedicine 2020; https://DOI.org/10.1016/j.eclinm.2020.100695.
- Atemfrequenz, flexikon.doccheck.com (Abruf: 18.1.2021)
- Atemfrequenz selber messen bei Lungenentzündung, www.cardiopraxis.de (Abruf: 18.1.2021)
- Strauß R, Ewig S, Richter K et al. (2014): The prognostic significance of respiratory rate in patients with pneumonia – a retrospective analysis of data from 705.928 hospitalized patients in Germany from 2010–2012. Deutsches Ärzteblatt; 111: 503-508, www.aerzteblatt.de (Abruf: 19.1.2021)
- S. Beck*, B. Laufer, S. Krüger-Ziolekund K. Möller (2020): Messung der Atemfrequenz mittels Drehraten -und Beschleunigungssensoren.
- Spirometire – die kleine Lungenfunktion, www.lungeninformationsdienst.de (Abruf: 18.1.2021)
- Strauß R, Ewig S, Richter K et al. (2014): The prognostic significance of respiratory rate in patients with pneumonia – a retrospective analysis of data from 705.928 hospitalized patients in Germany from 2010–2012. Deutsches Ärzteblatt; 111: 503-508, www.aerzteblatt.de (Abruf: 19.1.2021)
- Strauß R, Ewig S, Richter K et al. (2014): The prognostic significance of respiratory rate in patients with pneumonia – a retrospective analysis of data from 705.928 hospitalized patients in Germany from 2010–2012. Deutsches Ärzteblatt; 111: 503-508, www.aerzteblatt.de (Abruf: 19.1.2021)
- Messung der Atemfrequenz – Ergebnisse verschiedener Methoden schwanken stark, www.thieme.de (Abruf: 18.1.2021)
- Hieronymi U., Kramme R., Kronberg H. (2011) Respiratorisches Monitoring und Pulsoxymetrie. In: Kramme R. (eds) Medizintechnik. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-16187-2_41 (Abruf: 18.1.2021)
- S. Beck*, B. Laufer, S. Krüger-Ziolek, K. Möller (2020): Messung der Atemfrequenz mittels Drehraten -und Beschleunigungssensoren.
- Cosinuss GmbH (2020): Cosinuss°In-Ear Sensor – continuous vital signs measurements. Cosinuss GmbH, Kistlerhofstr. 60, 81379 Munich.
- Strauß R, Ewig S, Richter K et al. (2014): The prognostic significance of respiratory rate in patients with pneumonia – a retrospective analysis of data from 705.928 hospitalized patients in Germany from 2010–2012. Deutsches Ärzteblatt; 111: 503-508, www.aerzteblatt.de (Abruf: 19.1.2021)
- Meredith DJ, Clifton D, Charlton P, Brooks J, Pugh CW, Tarassenko L. Photoplethysmographic derivation of respiratory rate: a review of relevant physiology. J Med Eng Technol. 2012 Jan;36(1):1-7. doi: 10.3109/03091902.2011.638965. Epub 2011 Dec 20. PMID: 22185462.