Blood pressure
Synonyms and acronyms: RR (after the inventor of the blood pressure cuff Scipione Riva-Rocci), vascular pressure.
Blood pressure is the pressure exerted by the circulation of the blood on the vessel walls of the body and lung circulation.1 In everyday medical practice, this is usually understood to mean the arterial blood pressure of the large arteries.2 Along with other vital parameters, blood pressure provides information about a person’s health. In the long run, high blood pressure in particular can be dangerous to health.
Overview
| Unit | mmHg (millimetres of mercury) |
| Normal values | < 130/85 (adults) |
| Measurement methods | Invasive or indirect with blood pressure cuff according to Riva-Rocci. |
| Measurement sites | upper arm, wrist, ear, blood vessel (invasive measurement method) |
Definition: What is blood pressure?
The systolic blood pressure corresponds to the upper blood pressure value (in the above example: 120 mmHg) and indicates the maximum pressure in the heart ejection phase (tension phase = systole).
Systolic blood pressure
Der systolische Blutdruck entspricht dem oberen Blutdruckwert (im oben genannten Beispiel: 130 mmHg) und zeigt den maximalen Druck in der Herzauswurfphase (Anspannungsphase = Systole) an.
Diastolic blood pressure
The diastolic blood pressure, on the other hand, corresponds to the lower blood pressure value (in the above example: 80 mmHg) and indicates the minimum pressure in the heart filling phase (relaxation phase = diastole).
Blood pressure: normal values and deviations
Depending on age, different blood pressure values are considered “normal”. If there are deviations, the systolic and diastolic values are usually either increased or decreased together. However, there can also be a deviation of only one of the two values.3
Table 1: Blood pressure values- reference range:4
| Age | Systolic blood pressure (mmHg) | Diastolic blood pressure (mmHg) |
|---|---|---|
| 0 – 3 months | 70–86 | – |
| 3–12 months | 86–93 | 60–62 |
| 1–9 years | 95–101 | 65–69 |
| 9–14 years | 101–110 | 68–74 |
| 18+ years | ||
| optimal | <120 | <80 |
| normal | 120–129 | 80–84 |
| high normal | 130–139 | 85–89 |
Blood pressure too high / hypertension
Too high blood pressure is called hypertension.5
According to the European guideline, this is defined as blood pressure values of 140/ 90 mmHg or higher at rest. Since hypertension is common (average prevalence in adulthood: 50%)6 and is a strong risk factor for cardiovascular disease, it is clinically more relevant than low blood pressure.7 What makes the diagnosis and understanding of the disease particularly difficult is that the disease is asymptomatic in patients and is often diagnosed late. Treatment of hypertension is essential, however, because hypertensive crises with systolic blood pressure values > 180-230 mmHg can have serious consequences such as cerebral hemorrhage.
In the long term, multiple end-organ damage such as hypertensive retinopathy (eye), myocardial infarction (heart), stroke (brain) or nephropathy (kidney) can occur. A study conducted by Ebinger J. et al (2022) also showed that the risk of hospitalization is twice as high for hypertensives in the case of infection with the omicron variant of SARS-CoV-2 despite triple vaccination. It should be emphasized that hypertension alone, without other chronic conditions such as heart failure or diabetes, was responsible for a more severe course of covid-19 in the study.8
Both the start of treatment and the setting of the target blood pressure depend on the overall risk assessment. A change in lifestyle is essential for reducing blood pressure: alcohol and nicotine should be avoided as far as possible and in most cases additional weight loss is recommended. Drug therapy (ACE inhibitor/sartan and diuretic/calcium antagonist) can also be induced.9
Blood pressure too low / low blood pressure
Blood pressure values below 100/60 mmHg are considered too low and are called hypotension.
Possible symptoms of hypotension are mainly an increased pulse (tachycardia), dizziness, headache, pallor, involuntary muscle tremor, fatigue, lack of concentration and orthostatic dysregulation. Orthostatic hypotension is manifested by the dropping of blood into the legs when changing posture from lying to standing (orthostasis). The reason for this is that the body’s nerves cannot maintain the state of tension against gravity.10
Low blood pressure mainly affects younger people, especially women. In contrast to hypertension (see above), there is only a need for action such as drug therapy in the case of hypotension if the patient’s symptoms cause increased suffering. However, since low blood pressure can also be caused by diseases such as heart valve defects, anemia or adrenal dysfunction such as Addison’s disease, this should also be investigated in the long term. Measures such as sufficient fluid intake (2 – 2.5 liters per day), alternating showers, sauna sessions, physical training, sufficient night sleep and stays in regions such as the North Sea or the high mountains can help against low blood pressure.11
Hypotension can be categorized as follows:
- Primary hypotension: idiopathic (with no identifiable cause), in people with slender builds, often occurs along with physical inactivity.
- Secondary hypotension: endocrine (related to the endocrine system), cardiovascular, or drug causes (e.g., beta-blocker administration), hypovolemia (volume deficiency), or infection.
Regulation of blood pressure
The arterial blood pressure is intended to ensure a constant blood supply to all organs (organ perfusion). For this purpose, the body either makes adjustments to the arterial blood pressure or directly to the blood flow to the target organ.
The regulation of blood pressure takes place in the brain or in the transition to the spinal cord. Here, the formatio reticularis is located in the medulla oblongata. This extensive, diffuse neuron system in the brain stem controls the circulatory system and is in turn controlled by the hypothalamus.
In blood pressure and circulation regulation, a distinction is made between short-, medium- and long-term regulatory mechanisms, which in turn can influence vascular tone (vascular tension).12
Short-term regulation
The short-term regulation of blood pressure takes place within seconds.13 The resistance vessels, capacity vessels and the heart are responsible for this. The heart can change the blood pressure by adjusting the stroke volume14 and the heart rate.15
In the short term, blood pressure can be regulated by opposing adjustments of the parasympathetic and sympathetic nervous systems (see “The autonomic nervous system”). For example, if the blood pressure is elevated, the sympathetic nervous system is inhibited and the parasympathetic nervous system is activated. Stimulation of the parasympathetic nervous system causes the heart rate to decrease, the vascular tone of the veins to decrease and thus the central blood volume, the filling pressure of the heart and thus the stroke volume also decrease.16 The adjustment of sympathetic and parasympathetic nervous systems takes place via pressoreceptors or baroreceptors. They are located in the walls of the blood vessels and continuously register the blood pressure there.17
Medium-long term regulation
- Renin-Angiontensin-Aldosterone system (RAAS)
When systolic blood pressure falls to 100 mmHg or less, the enzyme renin is released in the kidneys. The enzyme now cleaves a large protein called angiotensinogen into angiotensin I. This in turn is cleaved into angiotensin II by the angiotensin-converting enzyme (ACE). Stimulated by angiotensin II, vasoconstriction of the arterioles (small arteries) occurs, leading to an increase in blood pressure. In addition, angiotensin II releases the hormones ADH from the pituitary gland and aldosterone from the adrenal gland. While the hormones angiotensin II and ADH retain natrium (salt) in the body, aldosterone also increases the excretion of potassium. The higher natrium content leads to the storage of water in the body, which in turn leads to an increase in blood volume in the body and thus to increased blood pressure.18
To lower blood pressure, the RAAS system is an ideal target for this reason: On the one hand, the cleavage of angiotensin I to angiotensin II can be pharmacologically influenced by ACE inhibitors. On the other hand, angiotensin II can be inhibited by so-called AT1 receptor antagonists (sartans).19Cardiovascular diseases, www.amboss.com (retrieved: 22.08.2022)
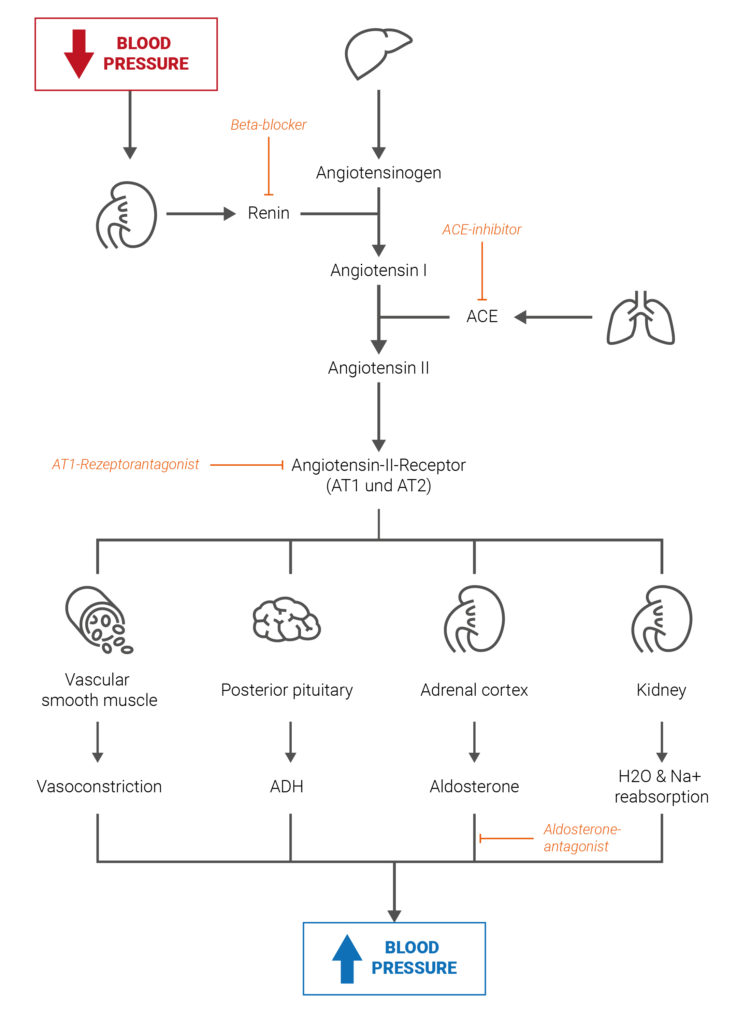
Fig. 1: Simplified schematic of the renin-angiotensin system and its influence on the regulation of blood pressure.
2. Gauer-Henry reflex
With the Gauer-Henry reflex, the release of the hormone ADH is adapted to the respective blood pressure situation. If the blood pressure rises, the ADH release in the thalamus20 is inhibited and as a result the kidney excretes more water.
If the blood pressure is too low, the mechanism works analogously in reverse.
3. Atrial dilatation reflex (using ANP)
The Gauer-Henry reflex influences the excretion of water from the kidneys in relation to the blood level of the heart. When the body volume is too high, the blood volume in the atria increases and is thus passively dilated. The reflex is mediated by B-sensors, which are called stretch sensors. If atrial dilation is increased, blood pressure is lowered by the release of the hormone ANP, which is produced in the heart. If more ANP is released, the kidney excretes more natrium and water and the parasympathetic tone is promoted while the sympathetic tone is inhibited.
What does blood pressure say about health?
Along with body temperature, blood oxygen saturation and heart rate, blood pressure is another important vital sign that helps to gain an even deeper insight into a person’s health. Deviations from the normal values, especially if they deviate significantly upwards, are often the cause of many cardiovascular diseases such as heart attacks and thus represent a major risk factor for health. But even a very low blood pressure can provide information about the current state of health.
Influence of diseases on blood pressure
Underlying diseases of the kidneys, thyroid or blood vessels can be the cause of high blood pressure in 10-15% of hypertensive patients. One of the causes, for example, is primary hyperaldosteronism (Conn’s syndrome). The body, or more precisely the adrenal gland, releases too much aldosterone here, which leads to an accumulation of water and sodium and thus to increased blood pressure.21 A study conducted in 2016 showed that 6% of the subjects with hypertension had Conn’s syndrome.22 Hyperthyroidism can also be responsible for high blood pressure. Another relevant factor in the development of hypertension is sleep apnoea syndrome, which is associated with nocturnal breathing pauses. It is reassuring to know that successful treatment of the underlying diseases can also treat hypertension.
There may also be a genetic predisposition to high blood pressure: In this case, there is an increased incidence of high blood pressure in the family and risk factors for high blood pressure are increased as a result.23
Secondary /side diseases due to high blood pressure
High blood pressure is an important risk factor for the development of many diseases or complications such as end organ damage.24 Some of the diseases are listed below:
- Diseases of the eye:
- Retinopathy (retinal disease that can severely affect vision)
- Blindness
- Cardiovascular diseases:
- Stroke
- Aortic aneurysm
- Heart failure
- Dementia
- Arteriosclerosis
- Coronary heart disease
- Cerebral hemorrhage
- Peripheral arterial occlusive disease (occlusion of arm or leg arteries, usually due to arteriosclerosis)
- Heart attack
- Cardiac arrhythmia with ventricular extrasystoles25
- Left ventricular hypertrophy (enlarged left ventricle of the heart)
- Diseases of the ears:
- Hearing loss (statistically higher risk for women)
- Tinnitus
- Mental illnesses/ diseases of the nervous system:
- Erectile dysfunction
- Cerebral circulatory disorder
- Depression (there is a higher risk of developing depression if blood pressure therapy with calcium antagonists or beta-blockers has been used)
- Diseases of the kidneys and urinary tract:
- Renal insufficiency
- Kidney failure
- Nephropathy with proteinuria (increased protein excretion)26
What influences blood pressure?
The level of blood pressure depends on both numerous physiological factors such as age, health status and gender, as well as external conditions, which are described in more detail below.
Blood pressure during the course of the day
Blood pressure is subject to large fluctuations during the course of the day, also known as the circadian blood pressure rhythm. Even before waking up in the morning, blood pressure rises continuously, there is a brief low at midday, while it then rises again from 4-6 p.m. and drops again significantly during the night.27 Renal hypertension is often characterized by hypertension at night – and thus by a disturbed circadian rhythm.
In addition, diabetes and hypertension (e.g. secondary forms of hypertension such as sleep apnoea) should also be considered when a disturbed circadian rhythm is detected. A large-scale meta-study showed that elevated blood pressure at night is a major risk factor for heart attack and stroke. They also concluded that blood pressure measurements taken during the day in hypertensive patients, for example in the doctor’s office, are less effective because night-time blood pressure is the most informative for the cardiovascular risk of the respective patient.28
Another study with 18.078 participants also showed that the targeted intake of blood pressure-lowering medication before a night’s rest significantly reduces the risk of cardiovascular disease.29 In contrast, too much lowering of blood pressure was observed in older people with silent reduced blood flow to the brain or heart.30
In addition, studies showed that lack of sleep or poor sleep quality can also increase blood pressure. The reasons for this are increased sympathetic activity and the release of cortisol in the adrenal glands.3132
Blood pressure in women and men
In the meantime, it is well known that illnesses can have different gender-specific courses. There are also differences in blood pressure between the male and female sexes: in general, it can be said that women’s blood pressure is lower than men’s until their menopause33 After the menopause, however, this changes. The evaluation of four cohort studies also showed that women had a 25% increased risk of cardiovascular diseases already at systolic blood pressure values of 100-109 mmHg (reference value: 100 mmHg), whereas this was only the case for men from 130-139 mmHg. In addition, the risk of stroke increased in women from a systolic blood pressure of 120 mmHg, while the same risk increased in men from 150 mmHg. Whether there should now be gender-specific standard values remains to be discussed. However, the study shows how important gender-sensitive medicine really is.34
Blood pressure in babies and children
The following table shows the blood pressure values divided by age:35
| Age | Blood pressure (mmHg) |
|---|---|
| Newborn | 60 / 40 |
| Infant | 80 / 60 |
| Toddler | 95 / 60 |
| Schoolchild | 100 / 60 |
| Adolescent | 110 / 70 |
| Adult | 120 / 70 |
| Elderly people | 150 / 90 |
In contrast to adults, there are no risk-adapted standard values for children, as these change with body growth. For this reason, they are defined in comparison to healthy control groups of the same size and age (percentile curves). If the blood pressure is above the 95th percentile, it is defined as “high blood pressure”.36
Higher than indicated blood pressure in children and adolescents is a growing health problem. If children are diagnosed with hypertension, they should be screened for cardiovascular or renal disease and diabetes mellitus. Effective treatments include weight loss (if overweight), a healthy diet low in salt, exercise and abstaining from alcohol and tobacco. The prevalence of hypertension in children aged 3-18 years is 3.6%.37 The majority of children diagnosed with hypertension also suffer from high blood pressure as adults.38
Blood pressure during pregnancy
Due to the hormonal changes, many bodily functions change during pregnancy. As a rule, blood pressure drops slightly, especially at the beginning of pregnancy, and the heart rate is increased. While low blood pressure does not normally pose any risks for the expectant mother and the child, too high blood pressure can be dangerous for both.39 A blood pressure of 140/90 mmHg is set as the limit value.
The following types of hypertension are distinguished in pregnancy (with frequency in percent in each case):
- Chronic hypertension: diagnosed before/during pregnancy (3%)40
- Pre-eclampsia: hypertension occurring during pregnancy with proteinuria (5-8%)41
- Gestosis: pre-eclampsia in women with chronic hypertension (20-25%)
- Gestational hypertension: high blood pressure that manifests after the 20th week of pregnancy and normalizes by 12 weeks after birth (6%).
Risk factors are considered to be general factors such as the presence of autoimmune or renal diseases, obesity, diabetes, older age or chronic hypertension. Multiple pregnancies, gestational diabetes and first births are also pregnancy-associated risk factors.42 The pathophysiological cause of hypertension in pregnancy is disturbed placentation43, which poses a risk to the fetus
If preeclampsia is not treated in time, it can lead to placental abruption and/or premature birth. A severe form of pre-eclampsia can also cause organ damage and seizures (eclampsia) in the pregnant woman.44 Since high blood pressure during pregnancy poses a great risk to the mother-to-be and the fetus, blood pressure should be checked regularly.
Blood pressure in old age
The risk of developing hypertension increases with age because the elasticity of the blood vessels continues to decrease. For this reason, three out of four people between the ages of 70 and 85 are hypertensive. In addition to the loss of elasticity, lifestyle habits in particular also seem to be causative for high blood pressure, as studies show that in indigenous people blood pressure remains constant even in old age.45 Treating blood pressure is essential, however, because high blood pressure in old age is also associated with an increased mortality risk. Attempts are made to adjust the systolic blood pressure to below 140 mmHg. Scientists from Ulm examined 1,100 participants and found out that the mortality risk is strongly influenced by the frailty46 of the test persons. While the optimal blood pressure in the fitter elderly subjects was 130 mmHg (related to mortality risk), it was surprisingly 160 mmHg in the very frail elderly. This study thus shows the importance of individual adjustment of blood pressure and that physical and mental fitness should be included in the treatment of hypertension.4748
Blood pressure during physical exercise
Blood pressure is generally higher during physical exertion, stressful situations or nervous strain. Under physical stress, the systolic blood pressure rises because the stroke volume of the heart increases – the diastolic blood pressure, on the other hand, remains approximately the same. However, the diastolic blood pressure also rises during maximum exercise. The reason for this is that maximum exercise leads to isometric muscle contraction and, as a result, peripheral vascular resistance increases sharply.49
However it is well known that physical activity can lower blood pressure in the long term: while it lowers the sympathetic tone, the vagus tone increases at rest. This lowers the heart rate and dilates the arterial blood vessels. For every kilogram of body weight lost, systolic blood pressure decreases by 1.5-2.0 mmHg and diastolic by 1.2-1.5 mmHg diastolic. Up to 160 mmHg (systolic), blood pressure can be normalized with three times a week exercise to a similar extent as with medication. If the blood pressure is above 160 mmHg, it must first be adjusted with medication to avoid dangerous blood pressure peaks. This is because high blood pressure can be seen as an important risk factor for sudden cardiac death during physical activity. Another study showed that every third person who died from sudden cardiac death was hypertensive. While a few years ago, low-intensity sports such as cycling, jogging or swimming were recommended and strength training was discouraged, more recent studies have shown positive effects on lowering blood pressure through strength training.
However, it is important to know that in the short term, high blood pressure first increases. The important thing here is that certain limits must not be exceeded. The appropriate choice of sport is also important, as certain types of sport trigger blood pressure spikes even in people with normal blood pressure levels. Studies show that regular exercise can greatly reduce the cardiovascular mortality risk in hypertensive patients.50 A prospective cohort study over 25 years concluded that the cardiovascular mortality rate was 70% lower in subjects with hypertension who were active in sports than in the control group who were inactive in sports.51 Blood pressure is generally higher during physical exertion, stressful situations or nervous strain. Under physical stress, systolic blood pressure rises because the stroke volume of the heart increases – diastolic blood pressure, on the other hand, remains approximately the same. Under maximum stress, however, this also rises.
Other influences on blood pressure
Blood pressure after a meal
After a meal, on the other hand, blood pressure is somewhat lower. The reason for this is that the human body is busy digesting and the digestive organs are therefore supplied with more blood. The blood volume of the body therefore decreases somewhat and so does the blood pressure. In order to avoid false results, blood pressure should not be measured immediately after a meal.52
However, if the blood pressure drops sharply after a meal, this is called postprandial hypotension. This can result in dizziness, lightheadedness and an increased risk of falling. It usually affects older people with high blood pressure or people who have damaged a center in the brain that controls the autonomic nervous system – i.e. in diseases such as Parkinson’s, Shy-Drager syndrome or diabetes. The reason for this is that blood pressure during digestion cannot be maintained by the blood vessels in other parts of the body. Eating small meals that are low in carbohydrates can help.53
Blood pressure and weather
It is often mistakenly assumed that high temperatures can lead to high blood pressure. In fact, the opposite is true: the high temperatures cause dilatation of the vessels and thus blood pressure drops. While hypotension is not dangerous for healthy people, it can cause serious problems for pregnant women and elderly people, as the supply of vital organs or the care of the child can no longer be guaranteed. If, on the other hand, the temperature drops, this becomes a problem, especially for hypertensive patients. The drop in temperature causes the vessels to contract further and the blood pressure rises, as a higher resistance has to be overcome.54
Blood pressure and coffee
Caffeinated drinks should not be consumed before a blood pressure measurement, as they can increase blood pressure by 10-20 mmHg in the short term. A higher increase in blood pressure after coffee consumption can be observed especially in people who drink coffee only occasionally – but with more frequent caffeine consumption, a habituation effect sets in.55 The question of whether the consumption of caffeinated beverages increases blood pressure is controversial. A systematic review and meta-analysis (n=172,567) concluded that drinking more than three cups of coffee a day compared to one cup or less was not associated with an increased risk of hypertension. However, a slightly increased risk was found with consumption of 1-3 cups daily.56
Blood pressure while lying down
When lying down, blood pressure is 3-10 mmHg higher than when sitting. For this reason, it is recommended that healthy, mobile people always take their blood pressure in a sitting position so as not to falsify the measurement results.57 However, in addition to the level of blood pressure, its stability is also of great importance. A study from 2006 showed that people with similar blood pressure levels when standing and lying down had twice the mortality rate of those whose blood pressure dropped significantly from lying to standing. In conclusion, unstable blood pressure can be regarded as a risk factor for cardiovascular disease.58
Blood pressure and pulse
The HARVEST study found that 15% of hypertension patients had a heart rate over 85 beats and 27% had a heart rate over 80 beats per minute. In addition, a high heart rate was shown to be a risk factor for developing hypertension during the course of the study.59
Heart rate variability (HRV), the variation in the time interval between two heartbeats, was also lower in hypertensives than in people with normal blood pressure levels. In addition, the likelihood of developing hypertension was higher when baseline HRV was lower than reference baseline.60
In contrast, some hypertensives have a consistently low resting heart rate. The so-called “baroreceptor reflex” is responsible for this: if the blood pressure rises, the parasympathetic nervous system is stimulated via the vagus nerve, the sympathetic nervous system is inhibited and thus the heart rate is lowered due to the negative chronotropic effect. If, on the other hand, the blood pressure drops, the parasympathetic nervous system is inhibited and thus the heart rate is increased.61
Measuring blood pressure
Since blood pressure is an important vital parameter for assessing the current state of health, it should be checked regularly. There are different types of blood pressure measurement available for this purpose.
Why measuring blood pressure is important
Regular and continuous blood pressure measurement is crucial because high blood pressure often has no symptoms. By detecting elevated levels early, appropriate therapeutic measures can be initiated to avoid serious cardiovascular complications such as heart attacks and strokes. In addition, continuous monitoring enables the effectiveness of therapy to be monitored so that medications and lifestyle changes can be adjusted. Recording blood pressure variability over the course of the day also helps to prevent phenomena such as the “white coat effect” or “masked hypertension”62. to identify what contributes to sustainably improved cardiovascular health overall.63 64
In emergency medicine, blood pressure measurement provides one of the most important pieces of information about a patient’s current circulatory condition. It makes it possible to quickly detect deviations from normal values that can indicate life-threatening conditions such as shock or sepsis. A blood pressure that is too low often signals circulatory collapse, while a value that is too high can indicate acute cardiovascular stress. Continuous monitoring of blood pressure in emergency medicine usually takes place invasively (hemodynamic monitoring via the artery or blood pressure measurement).65
How is blood pressure measured?
For measuring blood pressure – depending on the situation and requirements – different methods available.
Indirect blood pressure measurement according to Riva-Rocci
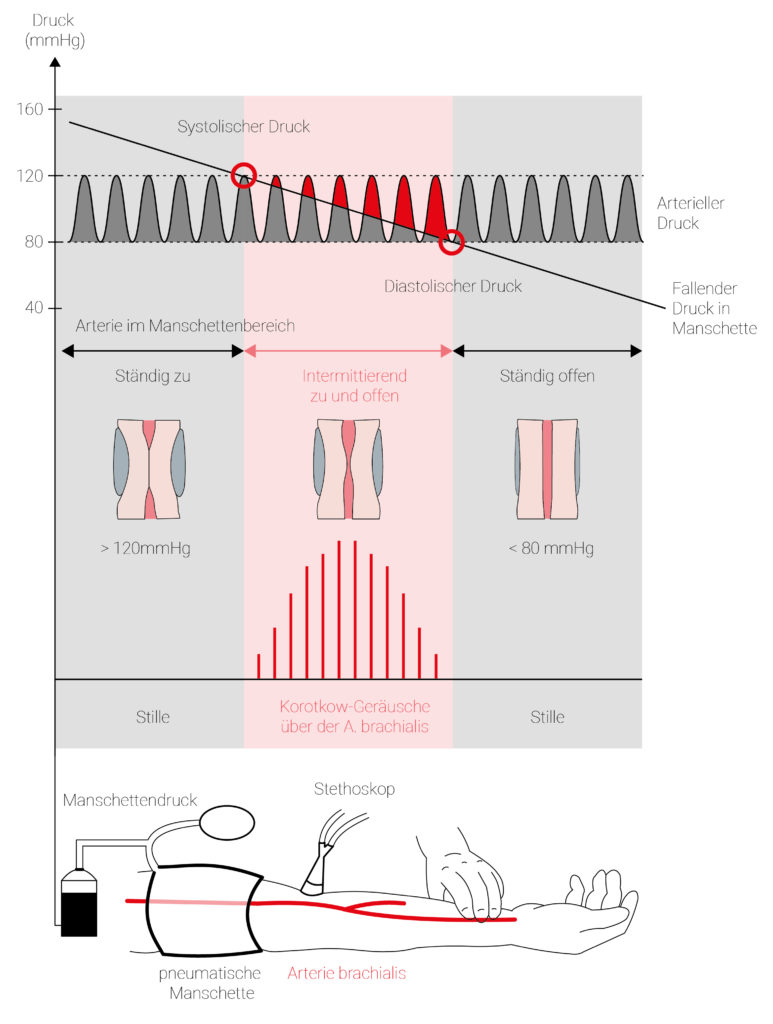
Fig 2.: Scheme for indirect, bloodless measurement of arterial blood pressure according to Riva-Rocci. Above the arterial blood pressure and the gradually decreasing cuff pressure, below the Korotkow sounds audible in the red area above the brachial artery. Below, sketch of the measurement arrangement.
Indirect blood pressure measurement according to Riva-Rocci uses either a blood pressure cuff on the upper arm and a stethoscope or an electronic blood pressure monitor (oscillometric blood pressure measurement66). Although these applications are somewhat less accurate than direct blood pressure measurement, i.e. the insertion of a measuring probe into the artery, they are used more frequently in everyday clinical practice because of their practicability.
The blood pressure cuff is applied to the upper arm, the valve must be closed beforehand. The stethoscope is placed in the crook of the elbow, it is pumped up quickly until the radial pulse is no longer visible.
Next, the valve is opened and the air is allowed to escape slowly. While the beginning of the sound represents the systolic value, the diastolic value is displayed when the sound disappears.
The principle of indirect blood pressure measurement works as follows: By compressing with a cuff, the blood flow in the brachial artery67 is stopped until the pressure of the cuff is greater than the systolic blood pressure and no flow noise can be heard. Air can escape through the valve opening. When the pressures of the cuff and the systolic blood pressure are equal, the blood can flow through the artery again. However, the blood does not flow continuously because the diastolic blood pressure is still lower than the cuff pressure. This results in a rhythmic alternation between blood flow (systole) and no blood flow (diastole). This alternation is the cause of the typical pulse-synchronous flow noises, also called Korotkoff noises. The cuff pressure continues to drop, while the valve remains open. If the values are lower than the diastolic blood pressure, no more flow noises are heard because the brachial artery remains open.68
Invasive blood pressure measurement
For continuous and precise blood pressure measurement, an invasive method is usually used, which is considered the current gold standard. A sensor is inserted directly into an artery via an arterial access. This allows the systolic, diastolic and mean arterial pressure as well as the arterial pressure curve to be recorded in real time.
Despite the high accuracy, this method also has disadvantages: complications are rare, but can include bleeding, hematomas or thrombosis. In addition, the arterial catheter must be inserted – even in emergencies – under sterile conditions to avoid infections.69
Where is blood pressure measured?
Normally, blood pressure is always measured on the same upper arm, at the wrist or in the ear canal, preferably while sitting. When measuring on the upper arm, the cuff must always be placed at heart level.
Influences on the measurement
It is important that the blood pressure measurement is always taken under the same starting conditions.
- To avoid measurement errors, a few things should be considered in advance:
The blood pressure measurement should always be taken at the same time, as blood pressure is subject to diurnal fluctuations.70 - Physical (e.g. pain) and/or emotional stress can strongly influence the blood pressure.
- Noise sources should be minimized and there should be no talking during the measurement.
- The size of the cuff should be appropriate for the patient’s upper arm circumference.
- Tight, constricting clothing should not be worn on the day of the measurement.71
- Caffeine and nicotine consumption can falsify the measurement results.
- Antihypertensive medication should not be taken until after the blood pressure measurement.
- The patient should not move and the feet should be placed side by side on the floor.
It is also important to note that the values measured in a doctor’s office are not always medically correct. One reason for this can be so-called white coat hypertension. Since the patient is excited when visiting the doctor, the blood pressure values are often higher than when measured at home.72
How does cosinuss° measure blood pressure?
cosinuss° determines blood pressure directly in the ear canal using a non-invasive, optical measurement technology. The sensor technology in the in-ear sensors is similar to how finger clip pulse oximeters work. A photoplethysmographic signal (PPG) is recorded, from which individual pulse waves are derived. From these, important vital parameters such as: Pulse rate and Oxygen saturation (SpO2) can be derived.
How does cosinuss° measure vital signs?
Author and reference information
About the authors
 |
Dr.-Ing. Johannes Kreuzer is co-founder and managing director of cosinuss°. He studied electrical engineering with a focus on medical electronics at TUM (Technical University of Munich, Germany). |
 |
Melanie Schade – M.A. Communication Studies and online marketing expert with a focus on health and science communication. |
Quellen / References
- Blood pressure, pschyrembel.de (retrieved:19.04.2022)
- Blood pressure, flexikon.doccheck.com (retrieved:19.04.2022)
- Blood pressure, flexikon.doccheck.com (retrieved:19.04.2022)
- Blood pressure,Table 1 pschyrembel.de(retrieved: 19.04.2022)
- Blood pressure, flexikon.doccheck.com(retrieved:19.04.2022)
- Arterial Hypertension, next.amboss.com (retrieved:20.04.2022)
- Blood pressure, flexikon.doccheck.com (retrieved:19.04.2022)
- Ebinger, Joseph E., et al. “Hypertension and excess risk for severe COVID-19 illness despite booster vaccination.” Hypertension 79.10 (2022): e132-e134.
- Arterial Hypertension, next.amboss.com (retrieved:20.04.2022)
- Hypotension, flexikon.doccheck.com(retrieved: 19.08.2022)
- Hypotension, when does low blood pressure become a problem, pharmazeutische-zeitung.de (retrieved:22.08.2022)
- Circulation regulation, next.amboss.com (retrieved:24.08.2022)
- Short-term and long-term blood pressure regulation Thieme, ViaMedici, viamedici.thieme.de (retrieved: 22.08.2022)
- The stroke volume is the amount of blood that flows through the body during a heartbeat.
- Circulation regulation, next.amboss.com (retrieved:24.08.2022)
- Circulation regulation, amboss.com (retrieved:20.09.2022)
- Baroreceptor, flexikon.doccheck.com (retrieved: 20.09.2022)
- Blood pressure regulation, msdmanuals.com (retrieved: 22.08.2022)
- Core region of the diencephalon.
- Hypertension causes, visomat.de (retrieved: 02.09.2022)
- Monticone, Silvia, et al. “Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice.” Journal of the American College of Cardiology 69.14 (2017): 1811-1820.
- Hypertension causes, visomat.de (retrieved: 02.09.2022)
- Secondary diseases hypertension, gesundheits-lexikon.com (retrieved: 02.09.2022)
- Benjamin EJ, Levy D, Vaziri SM et al.: Independent risk factors for atrial fibrillation in a population-based cohort: the Framingham Heart Study. JAMA 1994; 271(11):840-844
- Secondary diseases hypertension, gesundheits-lexikon.com (retrieved: 02.09.2022)
- fluctuations in blood pressure, herzstiftung.de (retrieved: 24.08.2022)
- Roush, George, et al. “Prognostic impact of clinic, daytime, and nighttime systolic blood pressure in 9 cohorts of 13,843 patients with hypertension: systematic review and meta-analysis.” Journal of the American Society of Hypertension 8.4 (2014): e59.
- Hermida, Ramon C., et al. “Asleep blood pressure: significant prognostic marker of vascular risk and therapeutic target for prevention.” European heart journal 39.47 (2018): 4159-4171.
- Antihypertensive chronotherapy: observance of the internal clock, www.aerzteblatt.de (retrieved: 24.08.2022)
- Bansil, Pooja, et al. “Associations between sleep disorders, sleep duration, quality of sleep, and hypertension: results from the National Health and Nutrition Examination Survey, 2005 to 2008.” The Journal of Clinical Hypertension 13.10 (2011): 739-743.
- Mansukhani, Meghna P., Naima Covassin, and Virend K. Somers. “Apneic sleep, insufficient sleep, and hypertension.” Hypertension 73.4 (2019): 744-756.
- On average, women are 51 years old at the beginning of their menopause.
- The end of unisex?, aerztezeitung.de (retrieved: 25.08.2022)
- praktischarzt.de (retrieved:24.08.2022)
- Simonetti, G. D., et al. “Bluthochdruck beim Kind.” Swiss Medical Forum. Vol. 10. No. 17. EMH Media, 2010.
- Riley, Margaret, and Brian Bluhm. “High blood pressure in children and adolescents.” American family physician 85.7 (2012): 693-700.
- Simonetti, G. D., et al. “Bluthochdruck beim Kind.” Swiss Medical Forum. Vol. 10. No. 17. EMH Media, 2010.
- Hypotension during pregnancy,apotheken-umschau.de (retrieved: 23.11.2022)
- Embryotox, hypertension, embryotox.de (retrieved:24.11.2022)
- >300mg/24h; increased protein excretion in urine.
- Embryotox, hypertension, embryotox.de (retrieved:24.11.2022)
- Maturation of the placenta.
- MSD Manual, pre-eclampsia and eclampsia, msdmanuals.com (retrieved: 24.11.2022)
- Blood pressure in old age – what can help? tk.de (retrieved: 28.08.2022)
- Decrease in physical fitness; associated with increased risk of falls.
- Blood pressure in old age – the main thing is to get it down? doccheck.com (retrieved: 29.08.2022)
- Kremer, Kaj-Marko, et al. “Systolic blood pressure and mortality in community-dwelling older adults: frailty as an effect modifier.” Hypertension 79.1 (2022): 24-32.
- Stress blood pressure, hypertoniezentrum.de (retrieved: 29.08.2022)
- Sport for hypertensive patients? aerztezeitung.de (retrieved: 29.08.2022)
- Engström, Gunnar, Bo Hedblad, and Lars Janzon. “Hypertensive men who exercise regularly have lower rate of cardiovascular mortality.” Journal of hypertension 17.6 (1999): 737-742.
- Blood pressure data, blutdruckdaten.de (retrieved: 29.08.2022)
- Postprandial hypotensio, msdmanuals.com(retrieved: 29.08.2022)
- When the weather weighs you down, deutsche-apotheker-zeitung.de (retrieved: 01.09.2022)
- Coffee and blood pressure: how many cups can I drink?, herzstiftung.de (retrieved: 29.08.2022)
- Zhang, Zhenzhen, et al. “Habitual coffee consumption and risk of hypertension: a systematic review and meta-analysis of prospective observational studies.” The American journal of clinical nutrition 93.6 (2011): 1212-1219.
- Blutdruck messen, apotheken.de (Abruf: 01.09.2022)
- Rose, Kathryn M., et al. “Orthostatic hypotension predicts mortality in middle-aged adults: the Atherosclerosis Risk In Communities (ARIC) Study.” Circulation 114.7 (2006): 630-636.
- Palatini, Paolo, et al. “Heart rate as a predictor of development of sustained hypertension in subjects screened for stage 1 hypertension: the HARVEST Study.” Journal of hypertension 24.9 (2006): 1873-1880.
- Singh, Jagmeet P., et al. “Reduced heart rate variability and new-onset hypertension: insights into pathogenesis of hypertension: the Framingham Heart Study.” Hypertension 32.2 (1998): 293-297.
- Baroreceptorreflex, flexikon.doccheck.com (retrieved: 01.09.2022)
- High pressure league: High blood pressure is not a trivial illness, https://www.hochdruckliga.de/pressemitteilung/bluthochdruck-ist-keine-bagatellerkrankung-besonders-tueckisch-die-maskierte-hypertonie-neue-broschuere-informiert (last accessed: February 28, 2025)
- German Heart Foundation: Measuring blood pressure: This is how you get reliable values https://herzstiftung.de/ihre-herzgesundheit/gesund-bleiben/bluthochdruck/blutdruck-messen (last accessed: February 28, 2025)
- High pressure league: Too variable in the long run – study discussion. https://www.hochdruckliga.de/nachricht/studienbesprechung-20230215 (last accessed: February 28, 2025)
- Jürgen Knapp, Michael Grabowski, Lorenz Weidhase, Michael Bernhard: Invasive blood pressure measurement – step by step. Cardiology up2date 2018; 14(04): 296-303 DOI: 10.1055/a-0770-3407
- Calculation of blood pressure by measuring the vibrations of the blood.
- Brachial artery: large arterial blood vessel in the region of the upper arm
- Blutdruckmessung, flexikon.doccheck.com (Abruf: 01.09.2022)
- Jürgen Knapp, Michael Grabowski, Lorenz Weidhase, Michael Bernhard: Invasive blood pressure measurement – step by step. Cardiology up2date 2018; 14(04): 296-303 DOI: 10.1055/a-0770-3407
- Gerloff, J. (1993). Blutdruckmessung. In: Paquet, KJ., Dieckhöfer, K. (eds) Allgemeine physikalische und klinische Untersuchungen. Springer, Berlin, Heidelberg. doi.org
- Blutdruckmessung, flexikon.doccheck.com (Abruf: 01.09.2022)
- Blutdruckmessung, tk.de (Abruf: 02.09.2022)