Pulse rate
Synonyms and abbreviations: Pulse, heart rate (HR).
In medicine, the term pulse rate refers to the number of pulses generated by the heart’s activity in the blood vessels during a specific unit of time (usually one minute). As a rule, the pulse rate coincides with the heart rate. Various factors, such as exercise, stress or certain diseases, can influence the pulse rate in the short or long term.
- Overview
- Definition: What is the pulse rate?
- Pulse rate: normal values and deviations
- What does pulse rate say about your health?
- What influences the pulse rate?
- Short excursion: The autonomic nervous system (sympathetic, parasympathetic)
- Pulse rate and respiration
- Relationship between body temperature and pulse rate
- Influence of sweating and dehydration on pulse rate
- Pulse rate and environment: humidity and altitude
- Pulse rate for women and men
- Pulse rate during sleep
- Pulse rate during sport
- Pulse rate and fat burning / fat burning heart rate
- Increased heartbeat after eating
- Pulse rate and overweight
- Pulse rate and smoking
- Change in pulse rate due to stress and other emotions
- Influence of diseases on pulse rate
- Measure heart rate and pulse rate
- How does cosinuss° measure vital signs?
- Related Articles
Overview
| Unit | beats per minute (min-1 or bpm). |
| Normal values | Newborn: 120-140 Infant: 120-130 Child: 100-110 Adolescent: 85-90 Adult: 60-80 Senior: 80-90 |
| Measurement methods | Manual (palpation) Electronic (electrocardiogram (ECG)) Optical (photoplethysmography (PPG)) |
| Measurement sites | Depending on the method, including wrist, finger, ear, neck, groin, popliteal fossa. |
Definition: What is the pulse rate?
The pulse describes the mechanical and rhythmic expansion as well as contraction of the vessel walls caused by cardiac activity and the pressure wave triggered by it. In a narrower sense, pulse is understood to be the vascular expansion of the arteries, which can be detected by touch or electronic measurement at specific regions of the body.1
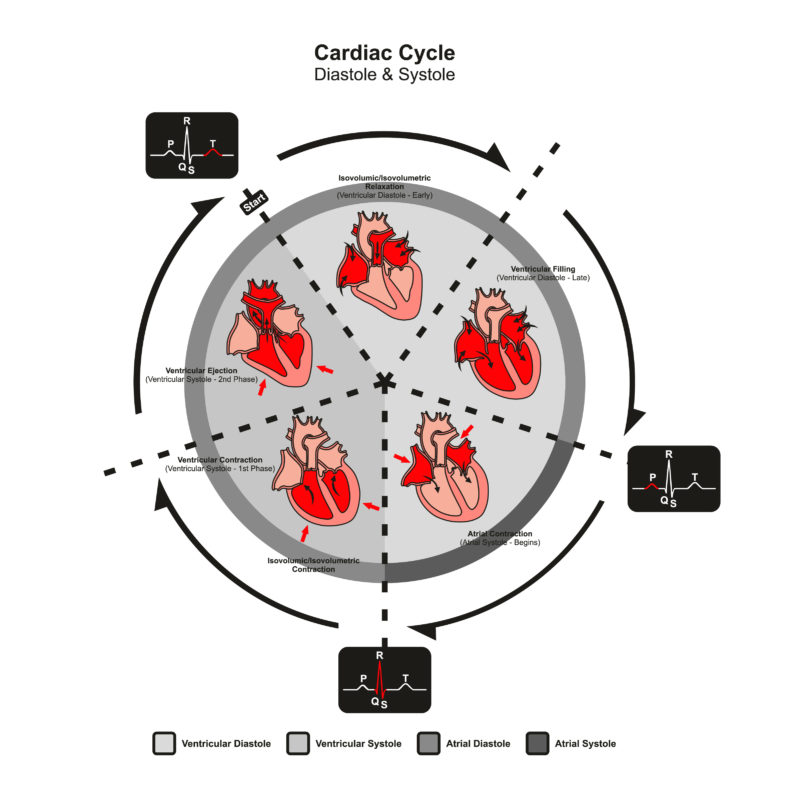
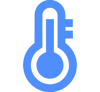
Fig. 1: Schematic representation of the heart’s action: The heart expels the blood by contracting intermittently. As a result, the blood does not flow evenly through the vessels, but in waves that can be felt as a pulse.
The pulse occurs in the arterial and venous parts of the vascular system. The arterial pulse, i.e. flowing from the heart into the body, provides information about heart rate, heart rhythm and blood pressure, among other things. The venous pulse, i.e. flowing back to the heart, on the other hand, is much weaker and has less clinical relevance. The pulsations visible in the blood capillaries, especially in the area of the skin, are called capillary pulses.2
Fig. 2: Schematic representation of the human circulatory system. Oxygen-rich blood travels from the lungs to the heart and from there to the body via the arteries. Oxygen-poor blood enters the heart via the veins and returns to the lungs.
Depending on the physical activity, the pulse can be divided into different types. At physical rest (lying or sitting), the so-called resting pulse or resting heart rate is normally between 60 and 80 beats per minute in healthy adults. The training heart rate is the optimal pulse rate for long-term endurance training. The maximum heart rate describes the pulse rate at maximum physical exertion.3
In clinical terms, the pulse can be assessed as follows:
- Pulse frequency: number of pulse beats per minute.
- Pulse rhythm: temporal sequence of the pulse beats.
- Pulse quality: type of pulse beat felt (soft, hard).
Radial pulse is the pulse in the area of the wrist on the thumb side (radial artery). Other pulse types, depending on their “measurement location”, include the temporal pulse, carotid pulse (neck), axillary pulse (axilla) and femoral pulse (groin).4 5
Briefly explained: pulse frequency, pulse rate, heart frequency and heart rate:
The pulse describes the mechanical and rhythmic expansion and contraction of the vascular walls caused by cardiac activity and the resulting pressure wave.
In medicine, the term pulse frequency refers to the number of pulses during a given unit of time (usually one minute). Pulse rate actually refers to the time between two beats. Thus, for a pulse frequency of 60 beats per minute, the average pulse rate would be 1 second.
In medicine, the term heart frequency refers to the number of electronically recordable heart actions during a specific unit of time (usually one minute). The heart rate indicates the time per heart action.
Colloquially, the terms pulse, pulse rate and heart rate are mostly used synonymously. In this text, we mainly use the word pulse rate unless explicitly referring to heart rate.
The pulse rate and heart rate are usually in agreement. However, deviations may occur if certain cardiac activities do not manifest themselves as a pulse wave in the vessels. This is the case, for example, with certain forms of arrhythmia.6 The difference between the heart rate and the peripherally measurable pulse rate is called a pulse deficit. Such a deficit occurs when a cardiac action does not affect the circulation (e.g. extrasystoles, atrial fibrillation) or the blood flow at the site of pulse measurement is unaffected by the heartbeat (peripheral disturbance, e.g. peripheral arterial occlusive disease).7
Pulse rate: normal values and deviations
A “normal” pulse rate depends on various factors. For example, in addition to the weather, time of day, medication or illnesses, the resting pulse rate is mainly dependent on physical condition and age. Gender also plays a role: women often have a slightly higher heart rate than men.8
| Age group | Pulses per minute |
|---|---|
| Newborns | 120 – 140 |
| Babies | 120 – 130 |
| Children | 100 – 110 |
| Adolescents | 85 – 90 |
| Adults | 60 – 80 |
| Seniors | 80 -90 |
The increased pulse rate of newborns and infants can be explained primarily by the high metabolic rates that decline with age.11
More on this topic:
Resting pulse – What it tells you
Pulse rate too high
If the pulse rate is too high, this is called tachycardia. In adults, the pulse rate is too high if it exceeds 100 beats per minute. For children, other limits apply depending on their age.12
Tachycardia can be caused, for example, by stress, anxiety, caffeine or various diseases (including thyroid disease or fever). However, a heart rhythm disorder can also be behind an excessively high pulse. In order to determine whether an elevated pulse is dangerous, it is important to clarify whether the measured pulse rate is permanently too high or is caused by a temporary external influence. If tachycardia or palpitations occur for no apparent reason, medical clarification should be sought.13 14 For example, according to a long-term study published in 2016, a permanently elevated resting heart rate is associated with an increased risk of heart attack and mortality.15
Mehr zu diesem Thema:
Reasons for high Heart Rate in Sports
Pulse rate too low
When an adult’s pulse rate is less than 50 to 60 beats per minute (bpm), it is called bradycardia. For children, other limits apply depending on their age.16
However, as a population-based cohort study published in 2016 suggests, for people without cardiovascular disease, a pulse below 50 bpm does not appear to be risky unless it causes discomfort.17 In addition, to assess whether a heart rate is too low and thus is pathological, the training condition of the heart as well as physical complaints and any heart diseases must be taken into account. Signs of a dangerously low heart rate include the following accompanying symptoms: Fatigue, dizziness, shortness of breath and/or fainting.18
A distinction is made between harmless and dangerous forms of bradycardia. In athletes, for example, so-called physiological sinus bradycardia (= without disease value) is harmless. Dangerous forms of bradycardia can be triggered by various heart diseases (e.g. heart attack, atrial fibrillation), hypothyroidism, hypothermia or potassium deficiency. In addition, a (too) low pulse rate can also be caused by certain medications, such as beta-blockers.19 20 21
What does pulse rate say about your health?
Although the pulse is a seemingly trivial physiological event, it allows conclusions to be drawn about the factors that determine it. Among other things, it provides information about the heart rate, the heart rhythm, the systolic rate of pressure rise as well as the blood pressure and the filling volume of the vessels.22
With the help of the pulse status, direct conclusions can also be drawn about the patency of the arterial system. To determine the pulse status, the arterial pulses are systematically measured manually at various points on the body and compared with each other. This is done in a lateral comparison or from proximal (closer to the center of the body) to distal (further away from the center of the body).23 In this way, for example, an inflammation of the vessels in the region of the aortic arch can be inferred, since in this case there is often an asymmetrical reduction of the pulses in the region of the upper extremities.24
In pulse quality, various pulse characteristics are assessed. These can provide information about the cardiovascular system. The pulse rate, rhythm, amplitude (size, strength, height), pressure increase and voltage of the pulse are examined and assessed. Depending on the pulse characteristics, various diseases or disorders of the cardiovascular system can be inferred. For example, a pulsus celer – a rapid pulse characterized by a rapid rise and fall in pulse rate – may indicate an unstable circulation or an aortic aneurysm. Despite the availability of diagnostic equipment (e.g. ECG), the pulse quality is often still checked manually by the physician, especially during the initial assessment of a patient. In this case, the first suspected diagnoses can often already be made.25 26 27
What influences the pulse rate?
How high the heart or pulse rate is depends on numerous internal and external physiological factors, age, gender, stress and psychological strain as well as life circumstances, which are described in more detail below.
Short excursion: The autonomic nervous system (sympathetic, parasympathetic)
The autonomic nervous system regulates a large part of the vital bodily functions, such as the heartbeat, breathing or digestion. It thus adapts our body to different living conditions, but cannot be directly controlled consciously. The autonomic nervous system is divided into two systems, which mostly work against each other (antagonistically):
- Sympathetic nervous system: this mainly has an activity-increasing function. In situations of stress and danger, it puts the body in a state of readiness to perform (“fight and flight”).
- Parasympathetic nervous system: This mainly has an activity-inhibiting function (“rest and digest”), although parasympathetic activity can also occur in stressful situations.

Fig. 3: Comparison of effects of sympathetic vs. parasympathetic nervous system on our organism.
Depending on the situation, the autonomic nervous system modifies the heart rate and its contraction force by activating the sympathetic and parasympathetic nervous systems. The aim of this modification is to increase or decrease the volume of blood pumped through the body per minute. In addition to influencing the heart rate, this can also be achieved by influencing the stroke volume. The sympathetic nervous system increases the heart rate, while the parasympathetic nervous system ensures a reduction. In addition, the two systems also influence the force of contraction, the conduction of excitation, the speed of relaxation, and the general excitability of the heart.
Depending on which system is activated, certain messenger substances or neurotransmitters are released in the body, which ensure that the heart rate is adjusted:
Pulse rate and respiration
Our breathing has an influence on our heart or pulse rate. The resulting fluctuation in the heart’s actions is called respiratory sinus arrhythmia (RSA). When we inhale, our heart rate increases, and when we exhale, it decreases.
Through breathing, it is thus possible for us to consciously influence the heart rate to a certain extent:
- If we breathe deeply and in a relaxed manner, the heart rate decreases because we take in more oxygen per breath.
- If we breathe shallowly, not enough oxygen can be taken in with one breath. As a result, the heart rate increases.
With the help of the measurement of the respiratory sinus arrhythmia, conclusions can be drawn about the vagal control (vagal = concerning the vagus nerve) of the heart. The measurement of RSA via pulse oximetry or ECG is thus an established standard procedure in functional diagnostics of the autonomic nervous system for checking parasympathetic activity.31
Relationship between body temperature and pulse rate
If the body temperature increases, e.g. due to sport activity or a high outside temperature, the heart rate increases. The reason: with an increased body temperature, the extremities are cooled down with the help of better blood circulation. At the same time, the muscles must be supplied with sufficient oxygen. In order to perform this additional work, the heart rate increases.32
Influence of sweating and dehydration on pulse rate
Excessive sweating and/or low fluid intake makes the blood “thicker”. The blood volume decreases, making it more difficult for the heart to transport the blood through the body. To compensate for this effect, the heart rate increases. In the case of dehydration, not only the pulse rate increases, but at the same time the blood pressure also decreases.33 34
Pulse rate and environment: humidity and altitude
At high humidity (from about 60%), the body’s thermoregulation is impaired because the evaporation of sweat decreases and it remains longer on the skin surface. To accelerate the slowed cooling process of the skin, the heart rate increases.35
Altitude also has an effect on heart rate: The lower air pressure ensures that the body can absorb less oxygen. To compensate for this effect, the breathing rate increases and thus also the heart rate (see also “Oxygen binding curve“).36
Pulse rate for women and men
Compared to men, women on average have an anatomically smaller heart. The structure and mode of action of the heart do not differ. The smaller size of the female heart means that less blood and therefore less oxygen is pumped through the circulatory system during a heartbeat. During physical exertion, this means that the female heart generally has to compensate for the increased oxygen demand of organs and muscles by beating faster. In addition to the smaller heart size and weight, women also have a smaller heart volume, stroke volume and cardiac output compared to men.
Table: Differences in cardiovascular parameters between women and men.37
| Cardiovascular parameters | Woman | Man |
|---|---|---|
| Heart weight | 250 – 300 g | 300 – 350 g |
| Heart volume | 500 – 600 ml | 600 – 800 ml |
| Stroke volume (at rest) | 40 – 50 ml | 70 ml |
| Cardiac output (at rest) | 3 – 5 l | 4 – 6 l |
| Heart rate (at rest) | 70 bpm | 60 bpm |
Pulse rate during sleep
During sleep, the pulse rate decreases, although this varies depending on the sleep phase.38 In addition, the respiration rate and blood pressure also decrease. Regular and sufficient sleep is important for the body to regenerate. In contrast, long-lasting sleep disorders can lead to an increased risk of cardiovascular diseases, in addition to psychological impairments, obesity and a weakened immune system.39 40
Pulse rate during sport
During physical activity, the muscle cells need more oxygen. To ensure this, the heart rate and the stroke volume increase. The pulse rate during sport therefore increases measurably and significantly.
Depending on age, a certain maximum heart rate should not be exceeded during sports. A rough rule of thumb for healthy adults is: pulse rate of 220 minus age. Thus, a healthy 40-year-old should not permanently exceed a pulse rate of 180, while a 60-year-old should only go up to 160 bpm. Important in this context, however, is how the pulse rate develops during sport. As a rule, the pulse rate rises gradually at the beginning of exercise and then falls slowly at the end. If, on the other hand, the heart starts to race or the pulse rate increases sharply at the beginning, this may indicate a disease-related cause.41
In the so-called overtraining syndrome, contrary to popular scientific publications, the heart rate is usually unchanged at rest. In the maximum range, however, the heart rate is slightly reduced (approx. 3-5 bpm).42 Heart rate variability (HRV), on the other hand, seems to be a suitable indicator of overtraining according to several studies.43
Like other muscles, the heart can also be trained. For example, endurance sports exert an influence on the resting pulse not only in the short term, but also in the long term. This happens because the heart gains mass over time and its blood volume per beat increases. As a result, it no longer has to beat as often to pump the required amount of oxygen through the body – the resting pulse rate therefore generally decreases in endurance athletes. An increase in heart mass also takes place in strength athletes, since recurring blood pressure peaks require increased cardiac output.44
More on this topic:
Pulse measurement during exercising
High Pulse When Exercising
Pulse rate and fat burning / fat burning heart rate
Often amateur athletes or people who want to lose weight talk about the “fat burning pulse”. What is meant is the optimal pulse to break down as much fat as possible. According to some studies and experts, however, it is important to clarify in this context that, on the one hand, fat burning and fat loss are two different things. Secondly, according to some authors, pulse-targeted training for fat loss does not exist. However, the existing training to enhance fat metabolism in turn is not meant for weight loss, but for more efficient muscular energy supply and thus for improving long-term endurance.
Contrary to what many assume, according to some authors the most efficient reduction of body fat percentage is not achieved with a moderate “fat burning pulse”, but with regular intensive training, such as interval training, strength training, intensive endurance training or circuit training. Such training variations burn more kilocalories per unit of time than moderate variations.
As a general rule for weight reduction, those who want to reduce their weight should pay attention to a negative energy balance, i.e. consume more energy than they take in through food.45 46 47
Note: Research on this topic is ongoing. Many of the aspects mentioned are controversially discussed by various authors and athletes.
Increased heartbeat after eating
After a large meal, the heart rate often increases for a certain period of time. The reason is the increased blood flow to the gastrointestinal tract required for digestion, so that more blood has to be pumped to this area directly after the meal.48
Pulse rate and overweight
Severe to very severe overweight (obesity) often leads to shortness of breath, especially during light exertion, because the lung volume is reduced by the existing fat cushions and the respiratory support muscles have to do more work. At the same time, oxygen consumption increases because more tissue has to be supplied with oxygen. These factors lead to an increase in heart rate.49
Pulse rate and smoking
Smoking can increase the heart rate by releasing the neurotransmitter norepinephrine. In this context, small amounts of nicotine, as ingested during smoking, increase blood pressure and heart rate. Excessive doses, on the other hand, lower the blood pressure and slow down the heartbeat.50
Change in pulse rate due to stress and other emotions
In states of stress, the sympathetic nervous system is particularly active (see “Short excursion: The autonomic nervous system“). In addition, catecholamines, a complex of hormones with an activating effect, are released. These cause the vessels in the muscles and other organs to dilate and the peripheral vessels to constrict. As a result, the heart rate increases. Emotions such as anxiety, anger, fear, surprise, joy, excitement or nervousness can also lead to an increase in heart rate.51
Influence of diseases on pulse rate
Various diseases can have a slowing or accelerating effect on the heartbeat.
Diseases such as anemia, hyperthyroidism (overactive thyroid) or hormonal fluctuations (e.g. menopause) can cause an increase in heart rate. Acute (infectious) diseases, such as a cold or flu, also represent enormous stress situations for the body, in which an increase in the pulse rate occurs due to increased body temperature or fever, among other things. Pulse-increasing diseases whose causes lie in the heart itself include cardiac arrhythmias, heart failure, inflammation of the heart muscle and heart valves, or cardiomyopathy.52 53
A reduction in the pulse is usually caused by diseases affecting the heart. The basis for healthy heart function is regular electrical impulses. If there are disturbances either in the formation of the electrical impulses or in their transmission, the heartbeat may slow down. These heart problems can be triggered by metabolic diseases such as hypothyroidism (underactive thyroid), among other things.54
Measure heart rate and pulse rate
How to measure pulse rate
The pulse rate can be measured manually or by means of special devices. The pulse rate can be measured manually or by “palpation” with the fingers at all points on the body where arteries run superficially. The best-known palpation site is in the area of the wrist (radial pulse). Electronic measurement of pulse rate takes place by means of electrocardiogram (ECG). For optical measurements, various devices and sensors can be used at different locations on the body. The most commonly used devices are earlobe and finger clips, smartwatches, fitness trackers or in-ear sensors.55
Manual measurement: how to check your pulse rate
For the manual measurement of the pulse rate, in addition to a hand as a “measuring instrument”, you need a display with a time recording possibility measuring in seconds. If you want to calculate the resting pulse rate, you should sit or lie relaxed for a few minutes beforehand.
In order to be able to measure the pulse itself, look for an artery that is running close under the skin and well palpable. The radial artery on the inside of the wrist on the thumb side and the carotid artery are particularly suitable for this purpose. The latter is located on both sides in the small pit between the larynx and the lateral neck muscles. Once a suitable spot has been found, place two to three fingertips (not the thumb!) on it with light pressure until you can feel the pulsating artery. Now count the incoming pulse waves for a quarter or half a minute and extrapolate the value to one minute (for a quarter minute take the value times four, for a half minute take the value times two).56
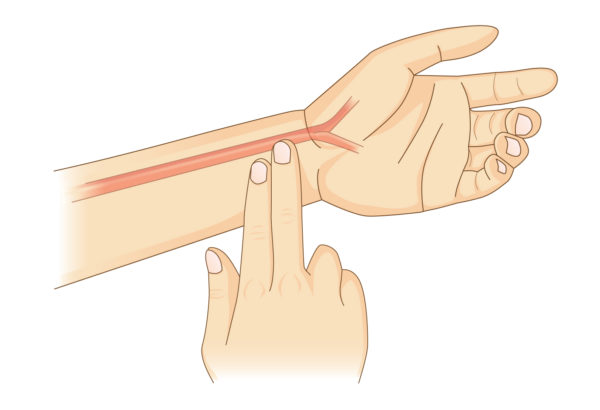
Fig. 4: Pulse measurement on the wrist with two fingers.
Electronic heart rate measurement: electrocardiogram (ECG)
In order for the heart muscle to contract, electrical excitation takes place. With each heartbeat, the heart muscles change their electrical properties. This creates an electric field that is conducted through the entire body. These voltage changes can be recorded with an ECG. Various conduction methods are available for recording: Unipolar and bipolar limb leads and chest leads. In bipolar limb leads, a total of three electrodes are attached to the right and left arms and to the left leg. On the basis of an ECG, the electrical activities in the individual sections of the heart can be displayed, but no statements can be made about the pumping capacity and contraction of the heart.57
Optical pulse rate measurement: photoplethysmography (PPG)
A PPG sensor is used to measure the pulse rate, which detects the changes in blood flow to the tissue. The sensor consists of a single green or red/infrared double LED light source and a light sensor (photodiode). The light emitted from the light source is either penetrated or reflected by the tissue and detected by the light sensor. As the tissue is perfused, the penetrating or reflected light intensity changes. In this way, the pulse can be detected. Today, such a PPG sensor is usually installed not only in pulse oximeters (e.g. finger clips, in-ear sensors) but also in fitness wristbands. In pulse oximetry, the functional oxygen saturation (SpO2) is measured in addition to the pulse rate.58
Briefly explained: Measurement of heart and pulse rate using ECG and PPG.
While the ECG measures the electrical activity of the heart, the PPG detects the change in blood flow to the tissue. An ECG thus directly measures the heart rate, while a PPG sensor detects the pulse rate.59
Where is the pulse rate measured?
The pulse rate can be measured manually, electronically and/or optically at all body sites where the arteries run superficially and can be “felt or seen” through the skin:60 61In the ear (external auditory canal)
- Earlobe
- Temple
- Neck
- Armpit
- Inside upper arm
- Elbow
- Wrist
- Finger
- Groin
- Back of the knee
- Ankle
- Arch of the foot
How does cosinuss° measure vital signs?
Related Articles
Author and reference information
About the author
 |
Dr.-Ing. Johannes Kreuzer is co-founder and managing director of cosinuss°. He studied electrical engineering with a focus on medical electronics at TUM (Technical University of Munich, Germany). |
Quellen / References
- Puls, flexikon.doccheck.de (Abruf: 01.10.2020)
- Kapillarpuls, flexikon.doccheck.de (Abruf: 01.10.2020)
- Puls, flexikon.doccheck.de (Abruf: 01.10.2020)
- Puls, flexikon.doccheck.de (Abruf: 01.10.2020)
- Radialispuls, flexikon.doccheck.com (Abruf: 29.09.2020)
- Pulsfrequenz, flexikon.doccheck.com, (Abruf: 28.10.2020)
- Pulsdefizit, flexikon.doccheck.com (Abruf: 29.09.2020)
- Welcher Puls ist normal?, www.herzstiftung.de (Abruf: 7.10.2020)
- Herzfrequenz, www.pschyrembel.de (Abruf: 9.2.2021)
- Pulsfrequenz, flexikon.doccheck.com (Abruf: 29.9.2020)
- Pulsfrequenz, flexikon.doccheck.com (Abruf: 29.9.2020)
- Herzrhythmusstörungen, www.amboss.com (Abruf: 28.10.2020)
- Welcher Puls ist normal?, www.herzstiftung.de (Abruf: 7.10.2020)
- Plötzlich schnelelr Puls, www.herzstiftung.de (Abruf: 28.10.2020)
- Custodis et al. (2016): Resting heart rate is an independent predictor of all-cause mortality in the middle aged general population. Clinical Research in Cardiology. 105. 601-612. 10.1007/s00392-015-0956-7, www.researchgate.net/publication/305514502 (Abruf: 28.10.2020)
- Bradykarde Herzrhythmusstörungen, www.amboss.com (Abruf: 01.10.2020)
- Klinisch herzgesund: Dann ist ein niedriger Puls meist harmlos. In: MMW – Fortschritte der Medizin, Ausgabe 3/2016, www.springermedizin.de (Abruf: 9.12.2020)
- Welcher Puls ist normal?, www.herzstiftung.de (Abruf: 7.10.2020)
- Reizbildungsstörungen, ruhr-uni-bochum.de (Abruf: 9.12.2020)
- Sommer, Philipp; Hindricks, Gerhard (2012): Herzrhythmusstörungen. In: Notfallmedizin up2date, www.thieme.de (Abruf: 9.12.2929)
- Bradykarde Herzrhythmusstörungen, www.amboss.com (Abruf: 01.10.2020)
- Puls, flexikon.doccheck.com (Abruf: 29.09.2020)
- Pulsstatus, flexikon.doccheck.com (Abruf: 28.10.2020)
- Klinischer Einführungskurs Innere Medizin, Internistische Kliniken USZ, Ressort Lehre USZ, 2020 www.usz.ch (Abruf: 28.10.2020)
- Pulsqualitäten, www.pschyrembel.de (Abruf: 3.12.2020)
- Klinischer Einführungskurs Innere Medizin, Internistische Kliniken USZ Ressort, Lehre USZ, 2020 www.usz.ch (Abruf: 9.12.2020)
- Pulsqualität, flexikon.doccheck.com (Abruf: 3.12.2020)
- Vegetatives Nerbensystem, www.amboss.com (Abruf: 8.10.2020)
- Eder, Ursula; Sperlich, Franz J. (2019): Das Parasympathikus-Prinzip: Wie wir mit wenigen Atemzügen unseren inneren Arzt fit machen. GRÄFE UND UNZER Verlag GmbH; 3. Edition.
- In this context, a five-year study conducted by the Klinikum rechts der Isar of the Technical University of Munich found that heart attack patients whose RSA was weaker were more likely to die within the observation period. In the studied individuals with low RSA, the probability of death at the end of the five-year period was almost five times higher than in those with more severe respiratory irregularities. The findings: conclusions about a person’s life expectancy could be drawn from heart rate and breathing rate.30Aufschlussreiche Unregelmäßigkeiten, www.mri.tum.de (Abruf: 8.12.2020)
- Thermoregulation, flexikon.doccheck.com (Abruf: 3.12.2020)
- Dehydratation, www.amboss.com (Abruf: 9.12.2020)
- Dehydratation, www.pschyrembel.de (Abruf: 9.12.2020)
- Sport unter besonderen klimatischen Bedingungen – am Beispiel der Olympischen Spiele und der Paralympics in Athen, Bundesinstitut für Sportwissenschaft (Hrsg.), 1. Auflage 2004 www.bisp.de (Abruf: 8.12.2020)
- Schommer, Kai; Bärtsch, Peter: Basiswissen für die höhenmedizinische Beratung. Deutsches Ärzteblatt (2011): 108(49): 839-48 (www.aerzteblatt.de, Abruf: 12.8.2020)
- Herz-Kreislauf-System, ruhr-uni-bochum.de (Abruf: 8.12.2020)
- Gürcan, Safiye (2004): Einfluß des Schlafes auf die Regulation des sympathischen und kardiovaskulären Systems junger gesunder Männer, Inauguraldissertation zur Erlangung der Doktorwürde der Universität zu Lübeck, www.zhb.uni-luebeck.de (Abruf: 8.12.2020)
- Schlaf – Medizinisches Fachwissen, www.lecturio.de (Abruf: 8.12.2020)
- Schlaf fürs Gehirn. In. UniPress 176, Februar 2019 / 43. Jahrgang www.unibe.ch (Abruf: 8.12.2020)
- Welcher Puls ist normal? www.herzstiftung.de (Abruf: 28.10.2020)
- Urhausen A, Kindermann W. (2002): Übertraining. Institut für Sport- und Präventivmedizin, Universität des Saarlandes, Saarbrücken, Deutsche Zeitschrift für Sportmedizin, Jg. 53, Nr. 4. www.germanjournalsportsmedicine.com (Abruf: 8.12.2020)
- Hottenrott, K. & Gronwald, T. (2014). Bedeutung der Herzfrequenzvariabilität für die Regenerationssteuerung. Leistungssport 44 (5) S. 9-13 (www.researchgate.net, Abruf: 5.2.2021)
- Herzgröße und Schlagvolumen von Untrainierten und Trainierten, ruhr-uni-bochum.de (Abruf: 7.12.2020)
- Moosburger, Dr. Kurt A. (2000): Fettverbrennung im Sport: Mythos und Wahrheit, Innsbruck, veröffentlicht in “Gesünder LEBEN“ 05/2000, letzte Überarbeitung 2015, www.dr-moosburger.at (Abruf: 8.12.2020)
- Fettverbrennungspuls, www.meinegesundheit.at (Abruf: 8.12.2020)
- Scharhag-Rosenberger F (2021): Fettstoffwechseltraining. In: Deutsche Zeitschrift für Sportmedizin, Vol. 63, Issue 12, Page 357-359, www.germanjournalsportsmedicine.com (Abruf: 23.2.2021)
- Aufbau & Funktion des Blutkreislaufs, www.internisten-im-netz.de (Abruf: 8.12.2020)
- Gabel, Doris: Wenn die Luft weg bleibt, www.ifb-adipositas.de (Abruf: 9.12.2020)
- Deutsches Krebsforschungszentrum (Hrsg.): Nikotin. Pharmakologische Wirkung und Entstehung der Abhängigkeit, Heidelberg, 2008 (www.dkfz.de, Abruf 7.12.2020)
- Sympathomimetika, www.amboss.com (Abruf: 8.12.2020)
- Herzrasen (Tachykardie), www.ratgeber-herzinsuffizienz.de (Abruf: 9.12.2020)
- Fieber, praxis-widderich.de (Abruf: 9.12.2020)
- Bradykardie, www.ratgeber-herzinsuffizienz.de (Abruf: 9.12.2020)
- Pulsfrequenz, flexikon.doccheck.com (Abruf: 29.9.2020)
- Wie messe ich meinen Puls? www.stiftung-gesundheitswissen.de (Abruf: 7.12.2020)
- Versuche zur EKG- und EMG Messung, www.uni-muenster.de (Abruf: 9.12.2020)
- Poklonskaya, Elena; Härter, Dipl.-Ing. (FH) Hendrik (2017): Wie die Optoelektronik in Fitnessarmbändern den Puls misst. In: Elektronik Praxis Online. www.elektronikpraxis.vogel.de (Abruf: 9.12.2020)
- Poklonskaya, Elena; Härter, Dipl.-Ing. (FH) Hendrik (2017): Wie die Optoelektronik in Fitnessarmbändern den Puls misst. In: Elektronik Praxis Online. www.elektronikpraxis.vogel.de (Abruf: 9.12.2020)
- Puls, flexikon.doccheck.com (Abruf: 9.12.2020)
- Puls messen, www.praktischarzt.de (Abruf: 9.12.2020)