Oxygen saturation
Synonyms and abbreviations: blood oxygen saturation, O2 saturation, sO2.
Oxygen saturation (sO2) refers to the percentage amount of oxygen in the blood. Among other things, it provides information about the functional capacity of the lungs and the effectiveness of oxygen transport in the blood. Oxygen saturation can be determined either outside the body via pulse oximetry or invasively with the aid of a blood gas analysis.
- Overview
- Definition: What is oxygen saturation?
- Oxygen saturation: Normal levels and deviations
- What does oxygen saturation say about health?
- Excursion: Oxygen dissociation curve21
- What influences blood oxygen saturation?
- Blood oxygen saturation measurement
- How does cosinuss° measure vital signs?
- Related articles
Overview
| Unit | % (percent) |
| Normal values | 95-99% (SaO2) resp. 73% (SvO2) |
| Measurement methods | pulse oximetry blood gas test |
| Measurement sites | pulse oximetry: finger, ear, heel (newborns) blood gas test: blood |
| Statements on health | amongst others function of lungs current blood flow oxygen uptake and metabolic activity of tissues cardiac output |
Definition: What is oxygen saturation?
Oxygen saturation describes what percentage of hemoglobin (Hb) is loaded with oxygen molecules.1 The oxygen inhaled via the lungs is absorbed by the hemoglobin and transported to the tissues via the bloodstream. There, the charged oxygen molecules are released to the cells.
The following types of oxygen saturation in the blood are distinguished:
- sO2 – oxygen saturation in general
- SaO2 – arterial oxygen saturation
- SpO2 – pulsoxymetrically measured oxygen saturation
- SvO2 – venous oxygen saturation
- SzvO2 – central venous oxygen saturation
- S⊽O2 – mixed venous oxygen saturation
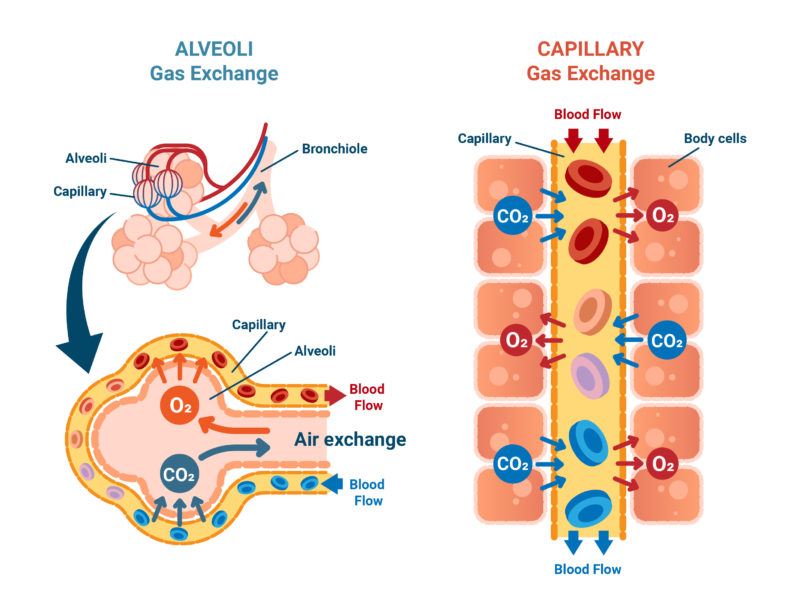
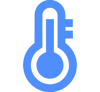
Fig. 1: Simplified representation of oxygen exchange from the lungs to the blood.
Hemoglobin (Hb) is a protein composed of four subunits. The most important function of hemoglobin is the transport of oxygen in the blood. It is predominantly found in the red blood cells (erythrocytes). In small amounts it is also found in plasma as free Hb bound to haptoglobin.
Oxygen is taken up from the air we breathe by hemoglobin in the small pulmonary vessels, transported throughout the body by the bloodstream, and delivered to the cells in the tissues. The oxygen-loaded hemoglobin is called oxyhemoglobin. When it has released all the O2 molecules, it is called deoxyhemoglobin. In its discharged form, it can absorb carbon dioxide and transport it back to the pulmonary vessels. There, the CO2 is released and exhaled again.
Fig. 2: Simplified representation of the loading and unloading of a hemoglobin with oxygen.
Depending on the loading or binding state, different hemoglobin variants are distinguished:
- Oxygenated hemoglobin (oxyhemoglobin – O2Hb): oxygen-bound hemoglobin (light red).
- Deoxygenated hemoglobin (deoxyhemoglobin – HHb): Hemoglobin without bound oxygen (dark red/purple).
- Carboxyhemoglobin (HbCO): carbon monoxide (CO) attaches to the oxygen binding site of heme.
- Carbaminohemoglobin: carbon dioxide (CO2) attaches to the N-terminal end of the globin chains.
- Glycohemoglobin (HbA1c): binding of glucose (sugar) to hemoglobin.
- Methemoglobin (MetHb): oxidation of the divalent iron of the heme group (Fe2+) to trivalent iron (Fe3+) (no more binding of oxygen possible).
Oxygen saturation: Normal levels and deviations
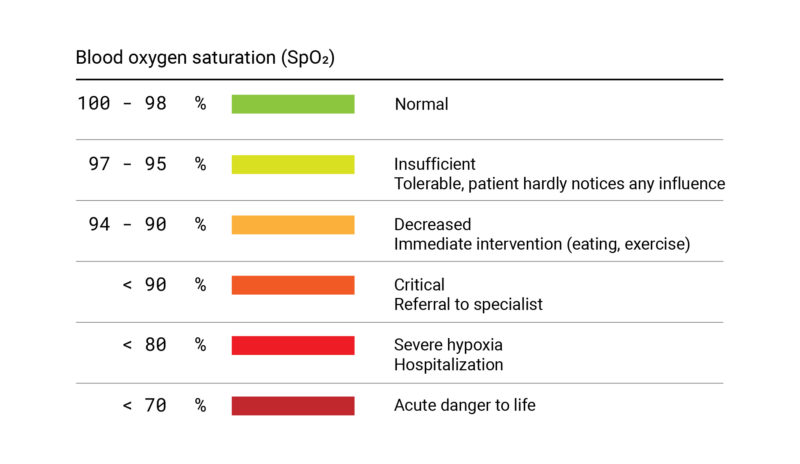
Fig. 3: Gradation of oxygen saturation levels in tabular form.
In a healthy adult, normal arterial oxygen saturation (SaO2) is 95-99%. When measured venously (SvO2) via blood gas test, the normal value of oxygen saturation is about 73%.4
Overview: Oxygen saturation standard values5
Pulse oximetry:
- Oxygen saturation (SaO2 or SpO2): 95-99%.
(to achieve a pulsoxymetrically measured oxygen saturation of approx. 98%, an oxygen partial pressure of approx. 100 mmHg is required)
Arterial blood gas test:
- pO2: 65-100 mmHg (9.5-13.9 kPa; age-dependent).
- pCO2: 32-45 mmHg (4.6-6.1 kPa; age-independent)
- pH: 7.35-7.45
- HCO3-: 22-26 mmol/L
- Base Excess: -2 to +2 mmol/L (or depending on the measurement method also ±3 mmol/L).
- Osmolality: 285-295 mOsm/kg H2O)
Blood oxygen saturation is not directly influenced by age or gender. The partial pressure of oxygen, on the other hand, is dependent on age. Thus, the partial pressure decreases with increasing age.6
Oxygen saturation increased / too high
A slight increase in blood oxygen saturation can be achieved by very rapid, deep inhalation and exhalation (hyperventilation). This simultaneously reduces the carbon dioxide (CO2) content.7
In addition, oxygen saturation may also be elevated during oxygen therapy. However, if there is already an adequate supply of oxygen in the blood, the additional addition of O2 can increase the risk of lung failure, heart attacks, cardiac arrhythmias and organ failure. Too much oxygen is toxic to the body and can cause inflammation, oxidative stress or constriction of blood vessels in the lungs, cardiovascular and nervous systems.
According to a meta-study8 (2018), supplemental oxygen administration already has harmful effects from a baseline value of 94-96%. According to the study results, the risk of patient death increases steadily with increasing oxygen saturation.9
Oxygen saturation too low
If oxygen saturation is too low, this is referred to as either hypoxemia or hypoxia. With hypoxemia the oxygen content in the arterial blood is reduced.10 Hypoxia is a lack of oxygen in the whole organism or in certain tissues. Symptoms may include anxiety and restlessness, dyspnea (shortness of breath), tachycardia (high heart rate), and increase in blood pressure.11
The following gradations of hypoxemia are made:12
Pulse oximetry:
- Mild hypoxemia (SaO2 = 90-94%, paO2 approx. 80 mmHg).
- Moderate hypoxemia (SaO2 = 85-89%, paO2 approx. 60 mmHg)
- High-grade / severe hypoxemia (SaO2 less than 85%, paO2 less than 50 mmHg).
Arterial blood gas test:
- Hypoxemic respiratory insufficiency: decreased partial pressure of oxygen (pO2).
- Hypercapnic respiratory insufficiency: Decreased partial pressure of oxygen (pO2) and increased partial pressure of carbon dioxide (pCO2).
- Latent respiratory insufficiency: Decreased partial pressure of oxygen (pO2) during exercise.
The following forms of hypoxia are distinguished:13
- Hypoxic hypoxia: partial pressure of oxygen (pO2) in arterial blood is too low.
- Anemic hypoxia: O2 transport capacity of the blood is reduced (e.g., due to a decrease in hemoglobin content or impaired O2 binding capacity).
- Ischemic or circulatory hypoxia (stagnant hypoxia): tissue perfusion is impaired (e.g., due to heart failure, blood vessel occlusion).
- Histotoxic hypoxia: cellular respiration is blocked by toxins.
There are many causes of low oxygen saturation: various lung diseases can lead to too little oxygen reaching the pulmonary alveoli (ventilation disorder). Diffusion disorders are also possible, in which the gas exchange between alveoli and capillaries is disturbed. In addition, diseases of the blood, such as anemia or hematopoiesis, cause impaired oxygen transport. Cardiovascular diseases such as heart failure cause insufficient oxygen supply to the organs due to vascular occlusion. In addition to diseases, environmental factors such as extreme altitudes can also lead to a decrease in oxygen saturation in the blood. Poisoning by e.g. medications, drugs or carbon monoxide also lead to a decrease in oxygen saturation.14
Silent Hypoxemia / Happy Hypoxemia
A special form of hypoxemia has occurred, particularly in connection with COVID-19: Many patients show no signs of shortness of breath or accelerated breathing despite severe hypoxemia with oxygen saturation levels as low as below 70%. This form of hypoxemia is particularly dangerous because, despite the absence of symptoms, decompensation of the lungs progresses rapidly and thus becomes life-threatening for patients.[/efn_note] 15
What does oxygen saturation say about health?
The measurement of oxygen saturation provides conclusions about the function of the lungs. By determining the saturation of the venous blood, the blood flow, oxygen uptake as well as metabolic activity of the tissue can be assessed. Peripheral oxygen saturation is also used to calculate arterial oxygen content (CaO2).16
Blood oxygen saturation is also frequently measured for continuous monitoring of patients who are under anesthesia during surgery or are receiving intensive care. For intensive care medicine, mixed venous or central venous oxygen saturation is particularly important, as it allows conclusions to be drawn about cardiac output.17
In emergency medicine, the measurement of blood oxygen saturation is used to obtain an impression of the patient’s oxygen content and respiratory gas balance.
In addition, oxygen saturation is measured to monitor the course of chronic lung diseases such as asthma or COPD.18
In the following cases, e.g. when certain symptoms occur or for various examinations, the measurement of oxygen saturation is useful from a medical point of view.
Overview: Indications for oxygen saturation measurement
Pulse oximetry
- Breath monitoring
- (Rapid) check of the oxygen supply
Blood gas test
- Early detection of cardiovascular or pulmonary diseases
- Gastrointestinal diseases
- Hemoglobin determination
- Hyperkalemia and hypokalemia
- Hyperventilation
- Control of pH value
- Control of respiratory therapy
- Renal failure
- Preoperative diagnostics
- Sepsis, shock, circulatory insufficiency
- Monitoring of the child during birth
- Monitoring of patients in intensive care and emergency medicine
- Unclear coma
- Suspicion of hypercapnia
- Follow-up of metabolic disorders
- Follow-up of chronic lung diseases
Excursion: Oxygen dissociation curve21
The partial pressure of oxygen is the pressure exerted by gaseous oxygen in the blood and is measured either in kilopascals (kPa) or millimeters of mercury (mmHg). The higher the partial pressure of oxygen (pO2) in the blood, the higher the oxygen saturation. This relationship is not linear, but s-shaped and can be represented in the oxygen dissociation curve (see Fig. 4). Thus, above a certain pO2, oxygen saturation increases only slightly.
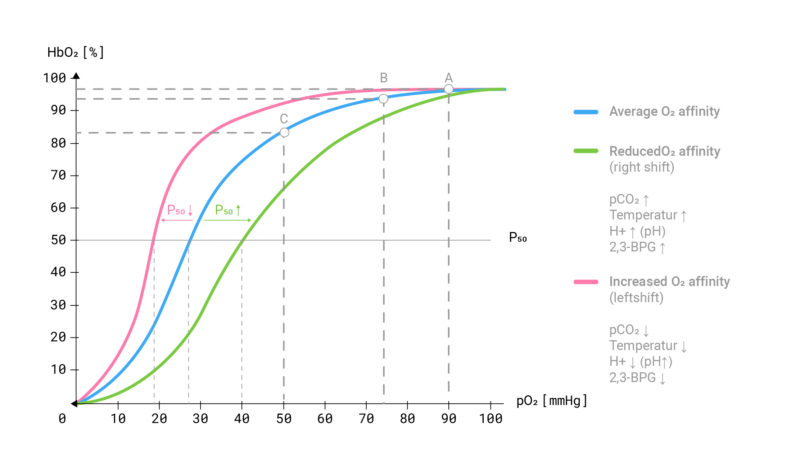
Fig. 4: The oxygen binding curve describes the relationship between the O2 saturation of hemoglobin and the partial pressure of oxygen (pO2) in the blood.
The shift of the oxygen dissociation curve to the left or right has many causes:
Left shift of the oxygen dissociation curve
A leftward shift means that at the same oxygen partial pressure, the hemoglobin can bind more oxygen. The oxygen is absorbed more easily from the alveoli and the bond between hemoglobin and oxygen becomes stronger. However, this has the consequence that the oxygen can be released less well into the tissues.
Causes for a left drift:
- Decrease in protons (leads to increase in pH: blood becomes more alkaline)
- Decrease in CO2 partial pressure
- Decrease in body temperature
- Decrease in 2,3-BPG (= 2,3-bisphosphoglycerate: regulates the binding strength of O2 to hemoglobin)
Example: A leftward shift of the oxygen binding curve is seen in hypothermia (hypothermia).22 For example, if you are in a very cold environment for a long period of time, your body temperature may be reduced, resulting in hypothermia of individual local areas of the body (typically the hands and feet) or even the entire body.23
Right shift of the oxygen dissociation curve
With a right shift, the bond between hemoglobin and oxygen is weaker. Oxygen cannot be absorbed as easily, but can be released into the tissues more easily.
Causes of a right shift:
- Increase in protons (leads to decrease in pH: blood becomes more acidic).
- Increase in CO2 partial pressure
- Increase in body temperature
- Increase in 2,3-BPG (= 2,3-bisphosphoglycerate: regulates the binding strength of O2 to hemoglobin)
Example: With increasing physical stress, there is a drop in pH due to an increase in protons in the blood (tissue acidosis). In addition, there is usually an increase in body temperature and an increase in CO2 partial pressure due to oxygen debt. These factors and the increasing concentration of 2,3-BPG cause a rightward shift in the oxygen binding curve and ensure that oxygen is more easily delivered to the tissues. However, hemoglobin no longer binds oxygen as strongly, which is why the respiration rate must increase. This relationship between pH, CO2 partial pressure with the oxygen dissociation curve is called the Bohr effect.
What influences blood oxygen saturation?
In addition to the influences on oxygen saturation or partial pressure already mentioned (pH, CO2 concentration, temperature, 2,3-BPG concentration), there are other factors that cause a change – usually a decrease – in arterial blood oxygen saturation. Some are described in more detail below.
Oxygen saturation during sleep
During sleep, human respiration changes:
- The respiratory drive decreases,
- the amount of air remaining in the lungs after exhalation is reduced due to the lying position,
- the relationship between lung ventilation and blood flow shifts.
In healthy people, these changes do not cause any problems compared to daytime breathing. In contrast, in patients with lung diseases such as pulmonary hypertension, they often lead to a lack of oxygen in the arterial blood.24
People with sleep apnea may also have a lower oxygen saturation at night due to frequent cessations of breathing, sometimes lasting up to two minutes. In severe cases of sleep apnea, the blood oxygen saturation of affected individuals is only about 70% at times.25
Oxygen saturation at altitude28
With increasing altitude, air pressure and O2 partial pressure (PO2) in the ambient air decrease, so that oxygen can no longer be absorbed as well by the hemoglobin. The result is a lower partial pressure of oxygen in the blood as well as a lower oxygen saturation. Via peripheral chemoreceptors, this reduced oxygen saturation is perceived in the body and hyperventilation is triggered. This slightly increases the alveolar PO2 and activates the sympathetic nervous system. The resulting increased heart rate compensates for the lower O2 content per heartbeat. However, this so-called acute adaptation cannot prevent the maximum oxygen transport and thus the maximum aerobic capacity (VO2max) from being restricted. Thus, an untrained person loses about 1% of his VO2max per 100m at an altitude of 1,500m, resulting in a power loss of 10% at 2,500m, 25% at 4,000m, and 65% at 8,000m.
Systemic blood pressure does not change significantly during acute adaptation at altitude because sympathetic activation and the direct vasodilatory effect of hypoxia neutralize in the peripheral circulation.
Endurance training at altitude can be used specifically to increase performance. The lower blood oxygen saturation at altitude causes a variety of adaptation reactions over a longer period of time:
- The number of erythrocytes increases (erythropoiesis) due to the release of the hormone EPO.
- The hemoglobin concentration increases, resulting in better oxygen transport.
- The respiratory and cardiac output increases.
- The capillaries also increase (capillarization), which enables better gas exchange.
Thus, altitude training increases aerobic performance. Gas exchange becomes more economical in the long run, as oxygen can be better absorbed and transported further. However, this altitude acclimatization takes time (about three weeks of continuous stay at high altitudes).29
Influence of diseases on oxygen saturation
Many diseases exert a negative influence on oxygen saturation and cause hypoxemia. The following is an overview of some diseases that can reduce oxygen saturation temporarily or permanently:30
Breathing restrictions/reduced breathing caused, for example, by
- Bronchospasm
- Head injuries
- Sleep apnea and snoring
- Stroke
- Shock
- Sepsis
- Oversedation
- Obstruction of airway or endotracheal tube due to secretion
Pulmonary diseases such as
- Acute respiratory distress syndrome (ARDS)
- Aspiration pneumonia
- Bronchial asthma
- Atelectasis
- Bronchitis
- Chronic Obstructive Pulmonary Disease (COPD)
- Covid-19
- Pulmonary embolism
- Pulmonary emphysema
- Pneumonia
- Pulmonary contusion
- Lung cancer
- Pneumothorax
Diseases of the blood such as
- Anemias
- Blood formation disorders
Cardiovascular diseases such as
- Heart attack
- Heart failure
Blood oxygen saturation measurement
How is oxygen saturation measured?
Oxygen saturation can be measured either outside the body via pulse oximetry or with the help of a blood gas test.
Pulse oximetry / pulse oximeter (SpO2)
Pulse oximetry is a non-invasive method for determining the oxygen saturation of the capillary blood (SpO2 value) and the pulse rate. Often, a clip with a sensor is attached to the fingertip or earlobe for measurement (pulse oximeter). The sensor consists of two parts: The light source emits red and infrared light alternately, which penetrates the skin. The light receiver (photodiode) records the light intensity and determines how much light of the different light colors was absorbed. The values measured in this way are usually very precise and correlate within a 4-percent deviation with the arterially measured oxygen saturation (SaO2). Pulse oximetry can only detect oxyhemoglobin or reduced hemoglobin, but not other hemoglobin variants such as carboxyhemoglobin or methemoglobin.31
Blood gas test
A blood sample is required for a blood gas test. This invasive method of measuring blood oxygen saturation is used to assess respiratory function and acid-base balance. It can be arterial or venous. The main parameters used to assess respiratory function are partial pressures for oxygen (pO2) and carbon dioxide (pCO2) and oxygen saturation (sO2). This can be used to assess respiratory insufficiency and ventilatory insufficiency. Important for the assessment of acid-base balance are pH, partial pressure of carbon dioxide (pCO2) and base excess (BE). The pH can be used to diagnose acidosis or alkalosis. The changes in pCO2 and BE can be used to determine whether they are respiratory or non-respiratory (metabolic, renal, intestinal) in nature.32
Where is oxygen saturation measured?
Depending on the measurement method, oxygen saturation is measured at different points, since arterial blood is generally equally saturated throughout the body. Thus, measurement is theoretically possible everywhere.
Pulse oximetry / non-invasive:
- Finger
- Earlobe
- In the ear (external auditory canal)
- Wrist
- Heel (for newborns)
Blood gas analysis / invasive:
- Blood sample
How does cosinuss° measure vital signs?
Author and reference information
About the author
 |
Dr.-Ing. Johannes Kreuzer is co-founder and managing director of cosinuss°. He studied electrical engineering with a focus on medical electronics at TUM (Technical University of Munich, Germany). |
Quellen / References
- Sauerstoffsättigung (sO2) www.pschyrembel.de (8.8.2020)
- Hämoglobin www.pschyrembel.de (Abruf: 12.8.2020)
- Hämoglobin www.amboss.com (Abruf: 13.8.)
- Sauerstoffsättigung (sO2) www.pschyrembel.de (8.8.2020)
- Pulsoxymetrie und Blutgasanalyse, www.amboss.com (Abruf: 6.8.2020)
- Pulsoxymetrie und Blutgasanalyse, www.amboss.com (Abruf: 5.11.2020)
- König, Peter; Lipp, Andreas: Lehrbuch für Forschungstaucher. Version: Juni 2007: 24. (ifm.uni-hamburg.de Abruf: 17.9.2020)
- Derek K Chu, MD et al.: Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. The Lancet (April 2018) Vol. 391, Issue 10131: 1693-1705. (www.thelancet.com, Abruf 12.8.2020)
- Auch eine Überversorgung mit Sauerstoff sollte vermieden werden www.lungenaerzte-im-netz.de (Abruf: 11.8.2020)
- Hypoxämie www.pschyrembel.de (Abruf: 12.8.2020)
- Hypoxie www.pschyrembel.de (Abruf: 12.8.2020)
- Pulsoxymetrie und Blutgasanalyse, www.amboss.com (Abruf: 6.8.2020)
- Hypoxie www.pschyrembel.de (Abruf: 12.8.2020)
- Hypoxie, flexikon.doccheck.com (Abruf: 17.9.2020)
- Tobin MJ, Laghi F, Jubran A. (2020): Why COVID-19 silent hypoxemia is baffling to physicians. Am J Respir Crit Care Med. 2020;202:356–60. https://doi.org/10.1164/rccm.202006-2157CP.
- Sauerstoffsättigung, flexikon.doccheck.com (Abruf: 6.8.2020)
- Sauerstoffsättigung, flexikon.doccheck.com (Abruf: 6.8.2020)
- Sauerstoffsättigung, www.netdoktor.de (Abruf: 6.8.2020)
- Pulsoxymetrie und Blutgasanalyse, www.amboss.com (Abruf: 6.8.2020)
- Blutgasanalyse (BGA) www.pschyrembel.de (Abruf: 11.8.2020)
- Wedel, Eva: Einfluss motorischer Belastung (Laufband) auf Blutgaspartialdrücke bei klinisch gesunden und respiratorisch erkrankten Pferden mit besonderer Berücksichtigung hypoxischer Zustände (2003) www.diss.fu-berlin.de, Abruf: 12.8.2020)
- Sauerstoffbindungskurve, flexikon.doccheck.com (Abruf: 2.11.2020)
- Hypothermie, flexikon.doccheck.com (Abruf: 2.11.2020)
- Hildenbrand, Florian F. et al.: Daytime Measurements Underestimate Nocturnal Oxygen Desaturations in Pulmonary Arterial and Chronic Thromboembolic Pulmonary Hypertension (2012) www.karger.com (Abruf: 12.8.2020)
- Gefährlicher Atemstillstand in der Nacht www.pharmazeutische-zeitung.de (Abruf: 12.8.2020)
- Sauerstoffsättigung (sO2) www.pschyrembel.de (8.8.2020)
- Meichsner, A.; Robel-Tillig, E.: Vergleich der postnatalen Sauerstoffsättigung und zerebralen dopplersonographischen Perfusionsparameter bei spontan und per sectionem geborenen reifen Neugeborenen. Klin Padiatr (2010): 222 (www.thieme-connect.com, Abruf: 12.8.2020)
- Schommer, Kai; Bärtsch, Peter: Basiswissen für die höhenmedizinische Beratung. Deutsches Ärzteblatt (2011): 108(49): 839-48 (www.aerzteblatt.de, Abruf: 12.8.2020)
- Höhensimulation: medizinische Wirkung, gairrit.com (Abruf: 10.2.2021)
- Abfall der Sauerstoffsättigung, www.msdmanuals.com (Abruf: 12.8.2020)
- Messung des Gasaustausches, www.msdmanuals.com (Abruf: 6.8.2020)
- Blutgasanalyse, lungenfunktion.eu (Abruf: 17.9.2020)